Earlier this year I had the pleasure of working with Rachel Bidder and others at Swansea Bay University Health Board on compiling information on Having a Tc‑99m Diagnostic Study whilst breastfeeding. Subsequently the information was shared in a presentation to the BNMS conference. In addition, the local team amended their information on MRI and CT to be more breastfeeding friendly.
The information from the Swansea team is reproduced here with their permission. If you have questions regarding expressing and storing, please contact your local breastfeeding team. My thanks to Rachel for allowing me to share this
Introduction
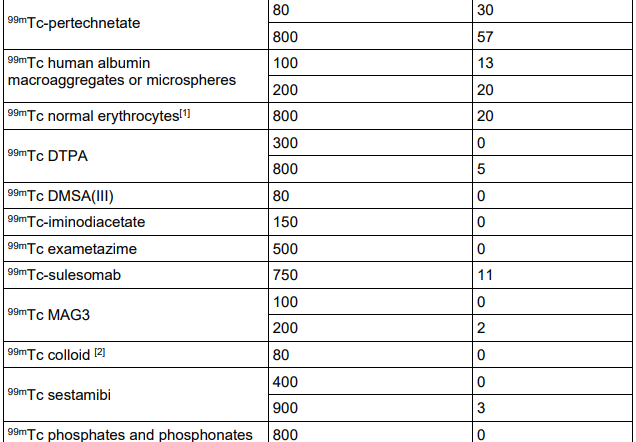
The vast majority of the radioactivity will be excreted via urine; however, a small amount will be excreted in breast milk. There are some precautions to follow to minimise the radiation dose babies receive. Radioactivity decays over time, meaning that not only will your body excrete it but the radioactivity itself will reduce. For Tc-99m, the radioactivity reduces by half every 6 hours, called the half-life. By following the advice in this leaflet (based on the ARSAC Notes for Guidance, 2022 and Drugs and Lactation Database, 2006), the radiation dose to your child from breastfeeding should be less than half of the annual natural background dose.
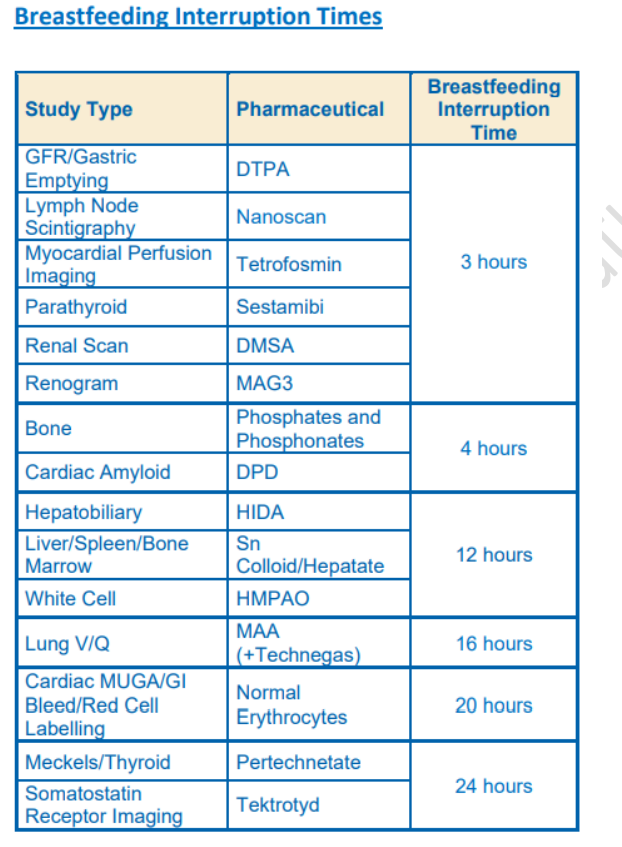
The disruption to your breastfeeding depends on the type of diagnostic study you are having. The interruption times given in this leaflet do not apply during the period of early lactation when colostrum is being secreted.
Before Your Appointment
All patients should ‘bank’ at least one feed before their appointment. Do this by expressing milk and storing it appropriately. Check the required breastfeeding interruption time for your scan using the table . It is recommended that you bank enough milk to feed your child over the length of this interruption period. If this is not possible for you then consider an alternative method for feeding your baby over this interruption period, such as using formula. Just before your appointment, you should feed your baby naturally.
After Your Appointment
You should not resume breastfeeding until after the total required period of interruption, as given for your study type in the table on the back of this leaflet. During this period of interruption, you should regularly express milk as fully as possible. This milk should not be used at this point. You can feed your baby during this time using a previously ‘banked’ feed. All milk expressed during the interruption time should either be discarded or stored in the freezer for at least 60 hours after your appointment. After 60 hours (10 half-lives), the radiation will have decayed to a safe level, and the stored milk can be used to feed (there is a small risk with this) or to bathe your baby as you please.
Once the interruption period has passed, you can continue to breastfeed your baby as normal.
Breastfeeding can be undertaken following subsequent pregnancies. Even if you have difficulty
expressing milk, the radioactivity will decay over time and will not be ‘stuck’ in your milk.
Summary

Reference
Notes for guidance on the clinical administration of radiopharmaceuticals and use of sealed
radioactive sources. Administration of Radioactive Substances Advisory Committee. Feb 2023
https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1137032/guidance-clinical-administration-of-radiopharmaceuticals-and-use-of-sealed-radioactive-sources-2023.pdf
“The patient should interrupt breastfeeding for a period of time to ensure that the effective dose received by the infant is less than 1mSv”
To tell a mother with a neonate not to breastfeed for a period of time risks her developing mastitis and will undoubtedly have an impact on her ability in the future to breastfeed
Healthcare professionals have a duty to protect the breastfeeding relationship to support the health of the patient and the breastfeeding infant
See also:
Drugs and Lactation Database (LactMed) https://www.ncbi.nlm.nih.gov/books/NBK501922/
Hale TW Medications and Mothers Milk Online access