I have recently written an article for ELACTA on a subject that causes so many problems. Just this week I received this question ” I have a 30 week prem baby, I didnt want to braestfeed so they gave me a single dose of cabergoline and the baby is having donor breastmilk. I’ve changed my mind and I would love to feed her. Can I give her the milk I have expressed today?” It is such a difficult question as we have so little data on the passage of cabergoline into braestmilk, the baby is very premature so has poor kidney and liver function and expressing to get a full supply is going to be a long hard journey. On the day of delivering such a tiny precious bundle, it is so hard to take in the implications of taking the drug
ELACTA is a European Journal for European Lactation Consultants. “Lactation & Breastfeeding” is also available in the UK as an electronic version for €8 per issue ( 4 annual editions) if you are not a member of ELACTA. Single Issues (elacta-magazine.eu)
PDF of the article can be downloaded
https://breastfeeding-and-medication.co.uk/wp-content/uploads/2023/01/Pharmacological-methods-of-weaning-versus-conservative-weaning.pdf

There are several different reasons why a mother may wish to wean her baby from the breast if we accept that weaning for the purpose of this article means as the cessation of breastfeeding rather than introduction of appropriate complimentary solid foods:
- Physiological natural weaning because the mother has decided that the time is right for them and their baby to stop breastfeeding and there is a natural reduction of milk supply.
- Unintentional weaning which may include ongoing supplementation or as a side effect of medication
- The prescription of medication to reduce lactation in the puerperium such as following a stillbirth or neonatal death, a baby to be adopted or where the mother has chosen not to breastfeed
- To rapidly cease lactation at a later period because of a medical diagnosis e.g., a diagnosis of cancer, or more rarely because of initiation of a medication which is incompatible with breastfeeding initiation of long-term methotrexate or lithium
- The use of supplementary or complimentary products to reduce lactation which may include perceived over-supply
- To discourage an older nursling who is reluctant to stop breastfeeding
- To stop lactation following a stillbirth or baby loss
Physiological weaning
For the majority of women weaning from the breast occurs gradually over a period usually after the introduction of appropriate complimentary solid foods (). As such under the influence of the Feedback Inhibitor of Lactation (FIL) supply diminishes slowly and without symptoms or discomfort or need for medication. As the baby breastfeeds less the feedback inhibitor lowers the production of milk.
Unintentional weaning
However, some 80% of lactations in the UK ceased before the baby was 6 months old and before the mother had planned to stop, usually because of lack of support and perceived low milk supply (McAndrew et al., 2012) In this case usually breastmilk feeds have been replaced by formula milk feeds so that breastmilk supply has gradually reduced and ceased altogether. This sadly can happen because a mother has misunderstood the way that milk supply is stimulated or that a short-term feeding plan involving top ups of formula milk or replacement of breastfeeds has been continued longer than may have been anticipated by the professionals. Not reaching the goals of breastfeeding been shown to be associated with feelings of loss and grief (Brown,2019) (.
Suppression of lactation in the puerperium when mother has chosen not to breastfeed
Some mothers of course choose not to breastfeed from birth because of personal wishes or ill health of mother or baby. In the past many of them were prescribed medication to dry up their milk. Oladapo& Fawole ) conducted a review of 46 controlled trials that randomised a total of 5164 mothers to receive the treatment under investigation, no treatment or another treatment (Oladapo & Fawole, 2019). The trials were generally of limited quality, and most were conducted among healthy women who chose not to breastfeed for personal reasons at hospitals in industrialized countries before 1980. Half of the trials involved bromocriptine which is no longer recommended for routine suppression of lactation and has indeed been withdrawn in USA by the FDA due to numerous maternal deaths.
Adoption
In the past many women whose babies were to be placed for adoption were offered medication to suppress lactation presumably to diminish the grief of the separation. In some cases, where limited contact with the baby is being maintained under supervision, mothers may choose to provide some breastmilk which can either be given as expressed breastmilk by the carer or directly by the mother feeding during contact. Anecdotally there have been reports to social services (personal communications to the author) where foster mothers have reported concerns that following maternal breastfeeds the baby appeared to have loose bowel motions and that the mother may be passing unacceptable substances via breastmilk. This exemplifies a misunderstanding of the difference between the bowel motions of breast and formula milk fed babies. There appears to be little research on the subject suggesting that long term expression is rare for babies given up for fostering and adoption. Whilst breastfeeding a baby who is to be adopted seems to be more common (Gribble 2006)
Stillbirth or neonatal death
For some mothers the choice to donate their breastmilk, following loss of their baby is a comfort and seen as a tribute to the baby’s memory (Jones, 2018) .
“When I gave birth to my stillborn daughter, I was given a dry up shot without them even mentioning donating to milk banks as an option. I would have LOVED donating my milk. ”“It’s funny, no one told me about milk donation. I don’t know how I knew about it. I learned when I was planning the C-section, I knew donor milk was an option, but didn’t know who donated it, never suspected I would become one who would be a milk donor.”
The side effects of cabergoline, used to stop lactation are not insignificant and it can precipitate depression, already a high risk after baby death in the puerperium.
Some mothers (personal communication to the author) were encouraged to not express their milk after sick, pre-term birth “just in case” their baby didn’t survive. In each of the cases, although limited in number, the mothers expressed regret that they felt that they had been excluded from caring for their baby.
Unintentionally lowering of milk supply due to medication
Drugs known to lower milk production as a side effect of use as medication are the combined contraceptive pill and the decongestant pseudoephedrine. Use to deliberately lower supply is not supported by research and effects vary with individuals. There have been no clinical trials on use for this purpose. Side effects of the drugs may be to raise the blood pressure of the mother and cause restlessness and irritability in the baby.
In one study of eight mothers (Aljazaf et al., 2003) a single dose of 60 mg pseudoephedrine was found to reduce the breastmilk supply by 24%. The reduction appeared to be more pronounced in those with later stage lactation defined as more than 60 weeks. The authors proposed that this may be due to a reduction in the production of prolactin although the reduction did not reach statistical significance with this small study population. Theoretically the reduction is also possible with the more frequently used phenylephrine although this hasn’t been reported in studies (Hale & Krutsch 2022, ) .
Dr Jack Newman has reported that bromocriptine and cabergoline are prescribed to overcome the symptoms of engorgement and mastitis sometimes on a routine basis (Newman, 2014) without the mother being aware of the potential effect on her long-term chances of successful breastfeeding.
Early post-partum use of the combined oral contraceptive pill has been shown to decrease milk supply in some women due to the oestrogenic activity. However, the reduction seen is not consistent and seems to vary from woman to woman. The studies available are very dated and evidence relies on anecdotal reporting by mothers and lactation specialists.
Other non-prescribed products used to reduce lactation
The herb sage has been reported to lower milk supply although without clinical research. In 2014 Eglash stated that “Sage is the most common herb used to reduce milk supply. Sage tea or extract made from the leaves is typically recommended, although there are no studies on the use of sage for hypergalactia and very few on its effect on the nursing baby. Sage tea may be prepared by steeping 1–3 g of dried sage leaves in a cup of hot water. The mother should be advised to just use one dose of the extract or 1 cup of tea and to observe the effect on her supply, as well as any behavioural change in the baby, over the next several hours. If she does not notice a difference in supply in 8–12 hours, then she can try another, stronger dose. Once she sees a response, she should just use it as needed. Often women will use one dose every 12 hours for 3 days to keep their supply down. Sage is known to have several side effects in high doses, including nausea, vomiting, and dizziness. It can induce wheezing, lower the blood sugar, and induce seizures, so high doses should be avoided in asthmatics, diabetics, and people prone to seizures. It is considered safe when used as a food.
In a 1998 Shrivastavet al studied the use of topical application of jasmine flowers was compared to bromocriptine to suppress lactation immediately after birth(. They reported that “The efficacy of jasmine flowers applied to the breasts to suppress puerperal lactation was compared to that of Bromocriptine. Effectiveness of both regimens was monitored by serum prolactin levels, clinical evaluation of the degree of breast engorgement and milk production and the analgesic intake. While both bromocriptine and jasmine flowers brought about a significant reduction in serum prolactin, the decrease was significantly greater with bromocriptine. However, clinical parameters such as breast engorgement, milk production and analgesic intake showed the two modes of therapy to be equally effective. The failure rates of the two regimens to suppress lactation were similar; however, rebound lactation occurred in a small proportion of women treated with bromocriptine. Jasmine flowers seem to be an effective and inexpensive method of suppressing puerperal lactation and can be used as an alternative in situations where cost and nonavailability restrict the use of bromocriptine.”
KellyMom reports that other herbs can be used to decrease supply but no evidence from research is supplied to support the statement. The herbs include Peppermint, Spearmint, Parsley, Chickweed, Black Walnut, stinging nettles, Yarrow, Herb Robert Lemon Balm, Oregano, Periwinkle Herb, Sorrel (KellyMom, 2018).
Normal consumption of the herbs as foodstuffs or drinking peppermint tea would not be likely to decrease supply.
Medication to reduce lactation
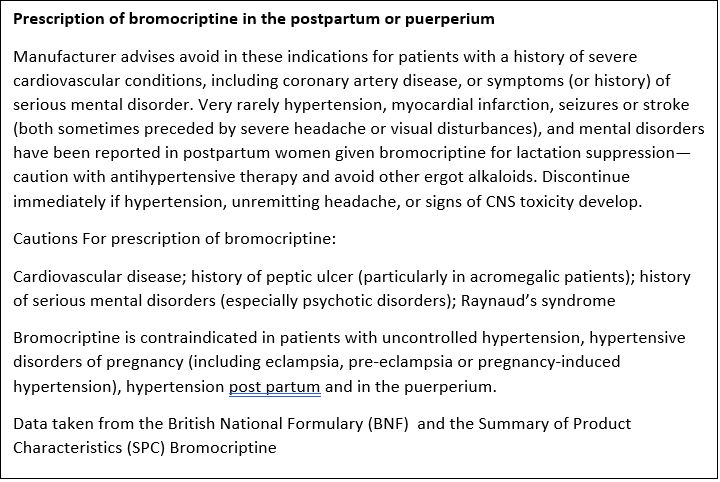
Bromocriptine
In 2015, the French pharmacovigilance program( Bernard) published a review of the adverse events associated with bromocriptine use to cease lactation. This group reported 105 serious adverse reactions including cardiovascular (70.5%), neurological (14.4%) and psychiatric (8.6%) events. There were also two fatalities: one 32-year-old female had a myocardial infarction with an arrhythmia, and a 21-year-old female had an ischemic stroke. (Hale & Kutsch 2022)(8)
Cabergoline
If a dopamine-receptor agonist is required to suppress lactation, cabergoline is preferred at a dose one mg, to be taken as a single dose on the first day postpartum. For the suppression of established lactation, a dose of 0.25mg is taken every 12 hours for two days for a total of 1mg (BNF 2022). However, this drug also has significant side effects, including headache, dizziness, fatigue or insomnia, orthostatic hypotension, oedema, nosebleed, dry mouth, inhibition of lactation, nausea, constipation, anorexia and weakness.
The manufacturer’s summary of product characteristics (Electronics Medicines Compendium SPC) ( states that:
“As with other ergot derivatives, cabergoline should not be used in women with pregnancy-induced hypertension, for example, preeclampsia or post-partum hypertension, unless the potential benefit is judged to outweigh the possible risk.
Serious adverse events including hypertension, myocardial infarction, seizures, stroke or psychiatric disorders have been reported in postpartum women treated with cabergoline for inhibition of lactation. In some patients the development of seizures or stroke was preceded by severe headache and/or transient visual disturbances. Blood pressure should be carefully monitored after the treatment. If hypertension, suggestive chest pain, severe, progressive, or unremitting headache (with or without visual disturbances), or evidence of central nervous system toxicity develop, cabergoline should be discontinued and the patient should be evaluated promptly.
In post-partum studies with cabergoline, blood pressure decreases were mostly asymptomatic and were frequently observed on a single occasion 2 to 4 days after treatment. Since decreases in blood pressure are frequently noted during the puerperium, independently of drug therapy, it is likely that many of the observed decreases in blood pressure after cabergoline administration were not drug-induced. However, periodic monitoring of blood pressure, particularly during the first few days after cabergoline administration, is advised”.
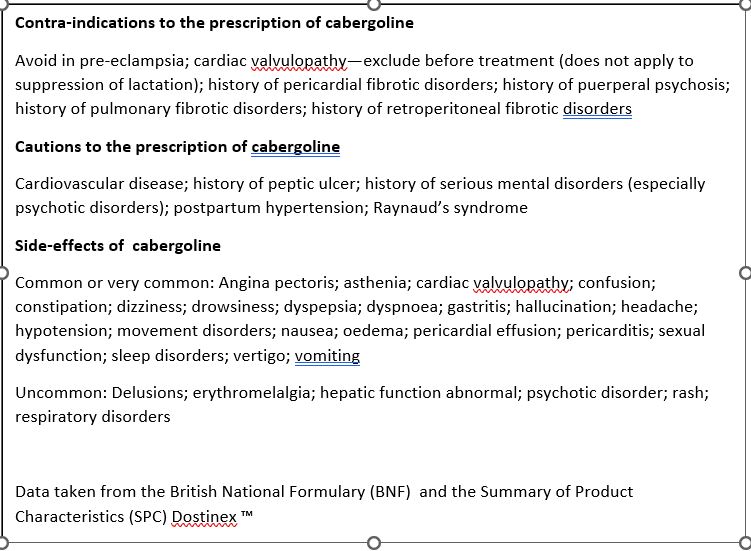
Cabergoline can also cause depression. They should be avoided if the mother has experienced pre-eclampsia. Both drugs can produce sudden onset sleep or excessive daytime drowsiness and driving should be avoided.
Although bromocriptine and cabergoline are licensed to suppress lactation, they are not recommended for routine suppression when women have decided not to breastfeed, or for the relief of symptoms of postpartum pain and engorgement that can be adequately treated with simple analgesics and breast support. Should the mother decide that she wants to continue to breastfeed after taking cabergoline caution is recommended as there are no studies on the effects on babies of the dose used to suppress lactation (Hale and Krutsh 2022). Elactancia suggests that “No untoward effects have been reported in breastfed infants of mothers who were treated (or erroneously had received medication) and decided to resume breastfeeding” whilst recommending waiting 3-7 half lives. The half life of cabergoline is 63-69 hours.
Weaning the reluctant nursling
Social media posts often have posts from mothers who are experiencing aversion to breastfeeding, sometimes around the time of menstruation, or because their babies are “nipple twiddling”. They report that they are desperate to stop breastfeeding whilst their nursling remains bonded and even reliant on breastfeeding. Discussions that they have felt unable to convince their little ones that milk has dried up are undermined when the nursling latches on and finds there is milk. They often question whether taking a medication to suppress lactation would be an option as a strategy of last resort!
“So, unless I can come up with a better plan, I need to dry my milk up. I bedshare with my 23-month-old (no other options), am a solo parent, and night nurse all night long (her choice, not mine). I planned to keep breastfeeding for as long as she wanted but I can’t nurse her at night anymore. I have no clue how to night wean her because I’m literally lying next to her all night long. So, I figured the easiest thing to do would be to dry my milk up with drug. “
Conclusion
In an ideal world it is better to allow the breastmilk supply to dwindle slowly, by dropping one feed at a time or expressing/feeding only when the breasts become uncomfortably full. It may however be necessary to speed up this process up, but it is still important to avoid blocked ducts and mastitis. It is possible to treat the breasts as in the early days of engorgement, using simple analgesics and cold savoy cabbage leaves in a firm but well-fitting bra. Or the mother can express just enough milk to remain comfortable, frequently changing breast pads, which may become soaked as milk leaks from the breasts. Restricting the fluids which the mother is drinking will not help the milk to dry up; nor will the use of laxatives to remove water from the body.
Whose choice should it be?
The choice should ultimately be that of the lactating mother having been provided with full information about the side effects of the drug, alternative methods of reducing supply and that this should be a final decision. So many times, mothers say that they have taken cabergoline but regret the decision and wish to return to breastfeeding, for example that formula isn’t suiting their baby. As with so many aspects of parenthood it isn’t always as easy a professionals might suggest.
References
- Aljazaf K, Hale TW, Ilett KF, et al. (2003) Pseudoephedrine: effects on milk production in women and estimation of infant exposure via breastmilk. Br J Clin Pharmacol. 56(1):18-24
- Bernard N, Jantzem H, Pecriaux C, et al. Severe adverse effects of bromocriptine in lactation inhibition: a pharmacovigilance survey. BJOG. 2015;122:1244-1251.
- Brown A, Why Breastfeeding Grief and Trauma Matter Pinter and Martin 2019
- Dr Jack Newman Facebook social media https://www.facebook.com/DrJackNewman/posts/the-use-of-cabergoline-dostinex-and-bromocriptine-parlodel-in-breastfeeding-wome/311003792384007/
- Eglash A. (2014)Treatment of maternal hypergalactia. Breastfeed Med. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4216483/pdf/bfm.2014.0133.pdf
- Elactancia online database https://www.halesmeds.com/monographs/60947?q=cabergoline
- Electronics Medicines Compendium SPC bromocriptine https://www.medicines.org.uk/emc/product/1202
- Cabergoline https://www.medicines.org.uk/emc/product/1691/smpc (accessed December 2022)
- Gribble, K.D. (2006) Mental health, attachment and breastfeeding: implications for adopted children and their mothers. Int Breastfeed J 1: 5
- Hale TW and Krutsch K Medications and Mothers Milk online access December 2022).
- Joint Formulary Committee. (2022). British national formulary. Accessed December 2022, fromhttps://www.medicinescomplete.com/#/browse/bnf
- Jones W Breastfeeding and Medication website lowering or stopping breastmilk supply https://breastfeeding-and-medication.co.uk/fact-sheet/breastfeeding-and-lowering-stopping-milk-supply
- KellyMom Herbs that may decrease milk supply https://kellymom.com/bf/got-milk/herbs_to_avoid/ Accessed December 2022
- McAndrew F, Thompson J, Fellows L, Large A, Speed M, Renfrew MJ (2012) Infant Feeding Survey 2010, Health and Social Care Information Centre
- Oladapo, O.T.; Fawole, B. (2009) Treatments for suppression of lactation. Cochrane Database of Systematic Reviews
- Shrivastav P, George K, Balasubramaniam N, Jasper MP, Thomas M, Kanagasabhapathy AS. Suppression of puerperal lactation using jasmine flowers (Jasminum sambac). Aust N Z J Obstet Gynaecol. 1988 Feb;28(1):68-71