As my youngest daughter nears the end of her pregnancy, I thought it was a good time to upload this information that I have been looking at for a while. I wrote the basis for a charity but it doesnt seem to have been used, so updating it and posting here. I dont have the same resources on drugs in pregnancy as I do in breastfeeding so please check UKTIS factsheets https://www.medicinesinpregnancy.org/Medicine–pregnancy/
https://breastfeeding-and-medication.co.uk/wp-content/uploads/2022/08/medicines-in-pregnancy-1.pdf
See https://www.sps.nhs.uk/articles/using-opioids-for-pain-relief-during-pregnancy/ for SPS information on opioids for pain relief in pregnancy
Medications are only prescribed in pregnancy after careful consideration of the risks and benefits to mother and baby. Thanks to a world-wide organisation The Organisation of Teratology Information (OTIS https://mothertobaby.org/about-otis/) who has a service in the UK (UKTIS http://www.uktis.org/), we have much more information on studies of medicine use in pregnancy and outcomes for mother and baby than we have ever had before.
This birth information page is not intended to provide advice on certain medication in pregnancy but to provide sources of information.
What medication should you take in pregnancy?
All pregnant women should take folic acid when trying to conceive and until 12 weeks of pregnancy. If the mother is on anti-epileptic medication, is obese (BMI >30), has a history of neural tube defects in a previous pregnancy, has coeliac disease, diabetes, sickle cell anaemia, thalassaemia, she or her partner have spinal cord defects, the dose should be increased to 5 mg daily.
There has been an unexpected increase over the past 15 years in the number of babies found to be suffering from rickets or symptoms of decreased bone mass which demonstrate poor levels of vitamin D (NICE PH11). Vitamin D deficiency is unusual in babies born at term to mothers with adequate vitamin D status. Some women enter pregnancy with low vitamin D levels. This may be due to:
• lack of exposure to sunlight due to wearing concealing clothing for cultural reasons.
• inadequate consumption of foods containing vitamin D e.g., oily fish.
• Inadequate consumption of dairy (prevalent particularly in adolescent girls)
• BMI greater than 30.
• Women who spend a lot of time indoors or use sun creams limiting the absorption of ultraviolet (UV) light.
• living in the northern hemisphere where levels of UV light are only sufficient to stimulate vitamin D production in the summer months; and
• having dark skin, which prevents absorption of available UV light in the UK climate.
Babies born to mothers with low vitamin D levels may be born deficient. It is advised that all pregnant women take 10mcg vitamin d daily throughout pregnancy https://www.nhs.uk/pregnancy/keeping-well/vitamins-supplements-and-nutrition/
Commercial vitamin products for pregnancy may also contain Omega 3 DHA, iron, zinc and vitamin B12
Is it safe to take medication whilst pregnant?
Drugs should be prescribed in pregnancy only if the expected benefit to the mother is thought to be greater than the risk to the foetus. All drugs should be avoided if possible, during the first trimester, although for may chronic conditions this may not be possible. Drugs which have been extensively used in pregnancy and appear to be usually safe should be prescribed in preference to new or untried drugs; and the smallest effective dose should be used. Few drugs have been shown conclusively to be teratogenic (harmful to an unborn baby) in humans, but no drug is safe beyond all doubt in early pregnancy (https://bnf.nice.org.uk/guidance/prescribing-in-pregnancy.html).
The tragedies wrought by thalidomide back in the 1960s have meant we are all more aware of the risk of drugs taken during pregnancy. Thalidomide was associated predominantly with limb defects, but it affected many other organs. A total of about 10,000 babies worldwide were affected. None of these abnormalities showed up in animal tests and it was believed to be so safe it was made available over the counter. In the original studies it was not possible to study enough pregnancies to identify a problem, although this became apparent when millions of mothers began to take it.
If you have a chronic medical condition which means that you need to continue to take drugs during your pregnancy, make sure that your doctor knows that you are pregnant (or ideally planning to become pregnant) so that they can try to avoid prescribing drugs which are known to be potentially harmful to an unborn child. For some people, having a chronic condition means having to take extra medication to support the pregnancy e.g., changing from the regular dose of folic acid of 400mcg to 5mg daily. If you are taking one of the drugs in the table below, please discuss the medication before considering pregnancy. If you are taking one of the drugs in the table below and fall pregnant accidentally or unexpectedly, please talk to your doctor as soon as possible – it is important that you don’t just stop taking the medication. If you are taking one of the drugs in the table below, please discuss the medication before considering pregnancy.
| ACE inhibitors e.g., enalapril, ramipril, perindopril | ACE (Angiotensin-converting enzyme) inhibitors may be used to treat high blood pressure and congestive heart failure. Women are normally advised to stop taking these when planning a pregnancy due to the risk of birth defects. |
| Statins e.g., simvastatin, atorvastatin | Statins are prescribed to lower cholesterol and so reduce the risk of a heart attack or stroke. Women are normally advised to stop taking these at least 3 months before conception occurs. |
| Anti-epilepsy Drugs (AED) | Most AEDs are teratogenic, although the risk is reduced when only one drug is used. Some AEDs are less likely to cause problems than others, but the risk to the unborn baby needs to be balanced with the risk of seizures in the mother which could harm both the mother and the baby. Women with epilepsy should therefore have a chance to discuss the choice of drugs and doses with a specialist when planning their pregnancy. Most women with epilepsy have normal, healthy babies and the risk of birth defects is low if the baby is not exposed to AEDs around the time of conception1 Pregnant women who are on any AEDs are usually recommended to take 5mg folic acid per day before becoming pregnant and through the first trimester, as it is thought that this may reduce the chances of a birth defect.1 Valproate medicines must not be used in women of childbearing potential unless the Pregnancy Prevention Programme is in place https://www.gov.uk/drug-safety update/valproate-pregnancy-prevention-programme-actions required-now-from-gps-specialists-and-dispensers See https://breastfeeding-and-medication.co.uk/fact-sheet/valproate-and-pregnancy https://breastfeeding-and-medication.co.uk/fact-sheet/carbimazole-in-women-of-childbearing-age https://breastfeeding-and-medication.co.uk/fact-sheet/topirimate-in-pregnancy-and-breastfeeding |
| Antibiotics | Many antibiotics including penicillins, erythromycin and cephalosporins are thought to be safe in pregnancy, but some are associated with problems. · Trimethoprim interferes with folate metabolism and so should not be prescribed in the 1st trimester. · Tetracycline can cause a yellow staining of the teeth and reduces growth of long bones. · Aminoglycosides such as gentamycin can cause deafness. |
| Warfarin | This is a blood thinning drug used to treat or prevent blood clots. It is not usually prescribed in pregnancy because it can cause foetal warfarin syndrome which is associated with a range of physical and sometimes mental problems. |
| Lithium | Lithium may be used in the management of bipolar disorder. If used in pregnancy, especially in the 1st trimester, it can sometimes cause an abnormality of the heart valves. This needs to be balanced against the risks to the mother of a relapse if she stops taking Lithium. If she is advised to stop Lithium or switch to a different drug this needs to be managed gradually. Women on lithium will usually be offered a high-resolution Ultrasound scan and foetal echocardiography at 18-20 weeks of pregnancy to check for heart defects. |
| Other drugs | Other drugs for chronic conditions include medications for diabetes, liver disease, heart conditions and mental health conditions. Please speak to your doctor or health care team if you take routine or regular medications outside of pregnancy. |
Risk of medication during pregnancy
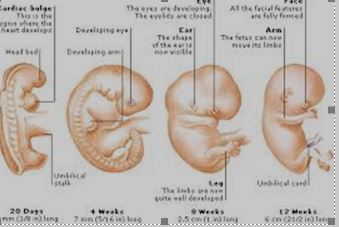
The risk of harm coming to a baby due to medication is greatest in weeks 3-11 after conception because this is when major organs are developing. During the second and third trimesters, drugs can affect the growth or functional development of the foetus, or they can have toxic effects on foetal tissues. Drugs given shortly before term or during labour can have adverse effects on labour or on the neonate after delivery.
It can be difficult to identify whether a drug has potential to cause harm to an unborn baby (teratogenic), because, if the problem is uncommon, a very large number of mothers would need to be studied for it to show up. Instead, drug side-effects are normally identified by collecting reports of problems via what is called the “yellow card” reporting system (https://yellowcard.mhra.gov.uk/). This data is analysed nationally and internationally so that any frequent side-effects can be identified and monitored. This monitoring is what has enabled data to be changed on the COVID 19 vaccination which originally was not recommended in pregnancy. Now we know that the programme is not only suitable for pregnant women but has also been seen as important (https://www.gov.uk/government/news/pregnant-women-urged-to come-forward-for-covid-19-vaccination)
What drugs are known to have a risk of causing birth defects?
To date, only 30 drugs have been shown to be teratogenic (harmful to an unborn baby). If you are planning a pregnancy and are taking any of these, you can discuss treatment options with your specialist, as a different drug or dose may be safer than your current one. If you have already become pregnant, speak to a specialist as soon as possible as there may be risks to stopping your medication abruptly which need to be balanced against the risk of birth defects if you continue. If you are taking one of these medications you should be using appropriate contraception https://assets.publishing.service.gov.uk/media/5c936a4840f0b633f5bfd895/pregnancy_testing_and_contraception_table_for_medicines_with_teratogenic_potential_final. pdf
The following is a good resource and a place to start when learning about drugs in pregnancy: https://www.newcastle-hospitals.nhs.uk/services/clinical-genetics/information-for healthcare-professionals/preconception-counselling/teratogenic-drugs/. There are also other sources, listed below which cover different stages of pregnancy.
Are there risks with non-prescription drugs or herbal remedies?
Over the counter medicines should be discussed with the pharmacist before purchase. The Patient Information leaflet (PIL) included in the packaging should state whether pregnant women are advised to avoid the drug. The leaflets on the BUMPS website can be really helpful https://www.medicinesinpregnancy.org/Medicine–pregnancy/UKTIS will discuss medication in pregnancy with professionals are unable to discuss medication with families.
Aspirin (or any preparations containing it) at a dose to be used as a painkiller (600mg four times a day) is not recommended for pregnant women because it is associated with an increased risk of stillbirth, low birth weight and possibly birth defects.4 However, it is sometimes prescribed in a low dose (75-150mg per day) to reduce the chance of miscarriage or pre-eclampsia amongst other reasons.
Herbal medicines have generally not been tested for safety, but they are subject to the “Yellow Card” reporting system in the same way as prescription drugs (https://yellowcard.mhra.gov.uk/) You should check with your midwife, pharmacist or doctor before taking any herbal medicines especially those containing multiple ingredients.
Foetal Alcohol Syndrome is seen in babies born to mothers who drink excessive amounts of alcohol, and no safe threshold amount can be defined (https://www.nhs.uk/conditions/foetal-alcohol-spectrum-disorder/)
Vitamin A intake needs to be limited in pregnancy so additional supplements should be avoided (https://www.nhs.uk/conditions/vitamins-and-minerals/)
Smoking also presents a risk to the developing foetus and should be avoided in pregnancy. Midwives can provide information in smoking cessation https://www.nhs.uk/pregnancy/keeping-well/stop-smoking
.Where do I find information on the drugs that I currently take?
If you have a medical condition that is being managed by a consultant or other specialist, they will discuss your current medication ideally before you become pregnant. Your GP may look in the BNF (British National Formulary), but this information may be limited. UKTIS has information available at https://www.medicinesinpregnancy.org/Medicine–pregnancy/.
There is a consortium set up by the MHRA working with many other organisations both within the NHS and third sector to provide evidence-based information on drugs in pregnancy (Safer Medicines in Pregnancy and Breastfeeding Consortium https://www.gov.uk/government/publications/safer-medicines-in-pregnancy-and breastfeeding-consortium)
Specialist information sources online:
● Guidance: Use of medicines in pregnancy and breastfeeding MHRA Jan 2021 https://www.gov.uk/guidance/use-of-medicines-in-pregnancy-and-breastfeeding
● BUMPS: best use of medicines in pregnancy https://www.medicinesinpregnancy.org/about-us/
● Mother to Baby https://mothertobaby.org/fact-sheets-parent/`
For most common medical conditions there are support groups with a webpage and/or a helpline.
References
1. RCOG Greentop Guide no 66 “Epilepsy in Pregnancy”, June 2016 2. Department of Health, UK Chief Medical Officer’s Alcohol Guidelines Review, January 2016
3. Collins E. Maternal and foetal effects of acetaminophen and salicylates in pregnancy, Obstet. Gynecol. 1981; 585 Suppl; 57S-62S 4. www.nice.org.uk/guidance/ph11/chapter/4-Recommendations#prescribing
5. Cochrane Review “Parenteral opioids for maternal pain management in labour”, July 2011
6. Tsamantioti ES, Hashmi MF. Teratogenic Medications. [Updated 2021 Aug 9]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK553086/
Further Reading
- Ainsworth SB (2014) Neonatal Formulary: Drug Use in Pregnancy and the First Year of Life 7th Edition Wiley Blackwell and BMJ Books
- Al-Zidan RN (2020) Drugs in Pregnancy: A Handbook for Pharmacists and Physicians 1st Edition
- Briggs G et al. (2021) Briggs Drugs in Pregnancy and Lactation: A Reference Guide to Fetal and Neonatal Risk 12th Edition. Lippincott Williams and Wilkins
- Jones W (2018) Breastfeeding and Medication. Routledge
- Priest J, Attawell K (1998) Drugs in Conception, Pregnancy and Childbirth Paperback
Schaefer C, Peters PWJ, Miller RK (Editors) (2014) Drugs in Breastfeeding and Lactation 3rd Edition. Ac