This information is largely taken from my book Breastfeeding and Medication (Routledge 2017)
Diarrhoea is defined as passing looser, watery or more frequent poo (stools) than is normal for you. It affects most people from time to time and is usually nothing to worry about. It can be distressing and unpleasant. It normally clears up in a few days to a week. It is often caused by bacteria in addition to vomiting but can occur alone. It may be part of another chronic condition e.g. inflammatory bowel disease.
Diarrhoea can lead to dehydration, involving excess water and electrolyte loss. Optimal treatment is oral rehydration. Acute diarrhoea is generally self-limiting and may be seen as the body’s attempt to rid itself of the infection. However, many people are unwilling to put up with the inconvenience of frequent, watery stools for more than a short period. Breastfeeding mothers may be concerned that their milk will dry up if their own symptoms of diarrhoea are not treated quickly. Mothers should be encouraged to drink according to thirst and to take rehydrating solutions in addition to anti-motility agents if there is excess fluid loss. Careful hygiene is important but there is no reason to stop breastfeeding if the mother has diarrhoea as she will pass on antibodies to the infection to her baby via the entero-mammary pathway.
Rehydration products are suitable for artificially fed infants in addition to formula milk during episodes of diarrhoea. Breastfeeding should be continued freely and should not be replaced by rehydration fluids. Exclusively breastfed babies have a very low risk of diarrhoea.
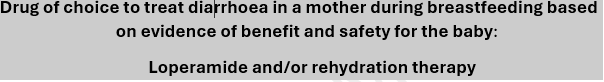
Rehydration therapy (Dioralyte®, Electrolade® Own Brands)
Rehydration solution sachets contain balanced levels of sugar and salts to correct the electrolyte and fluid balance. They would not affect breastfed babies as no significant levels would be passed into breastmilk. They may prevent dehydration of the mother with severe diarrhoea.
Compatible with use during breastfeeding as they only restore normal electrolyte balance.
Loperamide (Imodium®, Imodium Plus® (with simeticone), Own Brands)
Loperamide provides symptomatic relief of diarrhoea by inhibiting gut motility. Only small amounts are found in breastmilk as it is poorly absorbed (Nikodem and Hofmeyr 1992) making this a suitable drug to be taken by a breastfeeding mother. It is licensed to be given to children over the age of 4 years in syrup formulation at a dose of 1 mg three or four times daily for a maximum of 3 days.
For babies and children continued breastfeeding if applicable, and rehydration is generally recommended unless symptoms continue, as loperamide has been associated with toxicity and paralytic ileus.
Relative infant dose is quoted as 0.03% (Hale online access). The BNF states that amount secreted into breastmilk is probably too small to be harmful.
Compatible with breastfeeding as poorly absorbed from the gut.
References
Nikodem VC, Hofmeyr GJ, Secretion of the antidiarrhoeal agent loperamide oxide in breastmilk , Eur J Clin Pharmacol, 1992;42:695–6.
Codeine phosphate
The BNF states that the amount secreted into breastmilk is usually too small to be harmful; however, mothers vary considerably in their capacity to metabolise codeine and there is a risk of morphine overdose in infants (Koren et al. 2006). One death of an infant has been reported where the mother was an ultra-rapid metabolizer.
A study of two mothers found very low levels of free codeine and its metabolite morphine, in the plasma of breastfed infants whose mothers had taken a 60 mg dose of codeine. It was considered that such levels were sub-therapeutic and unlikely to cause respiratory depression (Naumburg et al. 1987). However concerns raised by Koren are important to take into consideration.
Relative infant dose quoted as 0.6% – 8.1% (Hale 2017 online access). Other preparations such as loperamide may be considered more suitable for a breastfeeding mother (see concern over codeine use under analgesics section).
Use loperamide as alternative if possible to control diarrhoea during breastfeeding as codeine may accumulate in baby and cause respiratory depression.
References
Koren G, Cairns J, Chitayat D, Gaedigk A, Leeder SJ, Pharmacogenetics of morphine poisoning in a breastfed neonate of a codeine-prescribed mother, Lancet, 2006;368(9536):704.
Naumburg EG, Meny RG, Findlay Brill JL and Alger LS. Codeine and morphine levels in breastmilk and neonatal plasma, Pediatr Res, 1987;21(4, pt 2):240A. Abstract.
Lomotil® Co-phenotrope (diphenoxylate plus atropine)
Co-phenotrope is a synthetic derivative of pethidine but has no analgesic effects. It reduces intestinal motility and is particularly useful in the control of faecal consistency after colostomy or ileostomy. It is rarely used purely as an anti-diarrhoeal drug any more. There is little information on its transfer into breastmilk and its use in lactation is not recommended. Unless there are compelling reasons to use co-phenotrope, loperamide is a safer option.
The BNF states that it may be present in milk.
Use loperamide as alternative if possible to control diarrhoea during breastfeeding as limited information on amount passing into breastmilk.