Home » Thoughts
Category Archives: Thoughts
Detox products and Breastfeeding
I am often asked about products, usually herbal, to detox and about breastfeeding afterwards. In general these products contain a combination of herbal laxatives and at least one diuretic . Basically the result is to make you pass more urine and develop diarrhoea to “cleanse” the system and usually to lose weight. There is a large risk that in doing so your milk supply will diminish too.
The data on the safety of the herbs in breastfeeding is often poor. I cannot provide data that these products are either safe to use and feed as normal or that they are unsafe – there is just is not enough data that I would be confident in using. Therefore I cannot help with information. The decision has to be your own or on the recommendation of a qualified herbalist who is willing to take professional responsibility.
Caffeine and Breastfeeding
Several questions have come up recently about caffeine intake and breastfeeding. With spending more time indoors we are probably all drinking more caffeinated beverages.
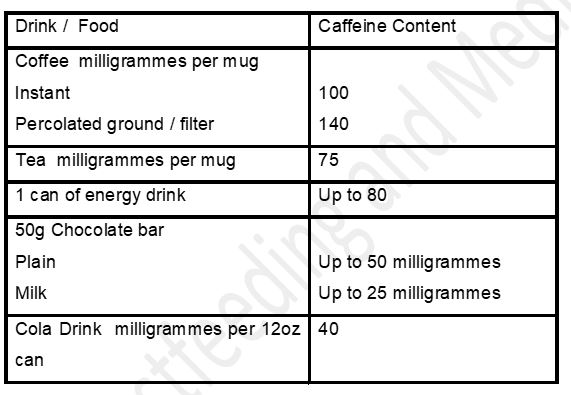
Most of us drink caffeine in one form or another. Women who drink a significant amount of caffeinated drinks who notice that their babies are jittery and restless, may find reduction in caffeine consumption leads to resolution of symptoms. This does not mean that all breastfeeding women need to restrict their consumption of tea and coffee A baby who appears restless may benefit from lowered caffeine intake by the mother but for the average consumption there is little evidence to support restricting intake. From research maternal consumption below 300 milligrammes a day should not cause issues for breastfed babies.
Extract reproduced from Breastfeeding and Medication 2018 by Jones W (Routledge, London)
See also https://www.e-lactancia.org/breastfeeding/caffeine/product/
Moderate coffee consumption does not produce significant levels of caffeine in plasma or urine of infants, and may be undetectable or below therapeutic levels in the neonatal period. (Blanchard 1992, Fulton 1990, Berlin 1984, Hildebrandt 1983, Bailey 1982, Rivera 1977)
Doses greater than 300 – 500 mg of caffeine daily can cause nervousness, irritability and insomnia in the infant (Santos 2012, Martin 2007, Clement 1989, Rustin 1989), as well as decreased iron levels in breast milk and anemia in the infant (Muñoz 1988). Also has been related to the Raynaud’s phenomenon in the nipple of nursing women. (McGuinness 2013)
One study found no problems in infants whose mothers consumed 500 mg of caffeine daily for 5 days. (Ryu 1985)
There is insufficient evidence on the recommended amount of caffeine during lactation. (McCreedy 2018)
Bowel cleansing before colonoscopy and breastfeeding
Just recently I have been contacted by several mothers who were told that they cant breastfeeding during the 24 hour period of bowel prep prior to a colonoscopy or for 24 hours following the procedure under sedation. This is not supported by research and understanding of the pharmacokinetics of the drugs used. It is also a potential risk in that the mother may develop blocked ducts or mastitis necessitating antibiotics if she is unable to express her milk, or in many cases hasn’t been advised to! Not all babies will drink from a bottle so may become dehydrated. Some babies are allergic to cow’s milk protein and may be compromised by 3 days of artificial formula. Hence this fact sheet on the bowel preparations generally used.
It is acceptable to breastfeed as normal during bowel prep. The mother should drink freely of the allowed clear fluids. Someone may be needed to look after the baby during rapid need to evacuate bowels – unless you have taken these products you cant begin to understand the urgency!
PDF of information available
https://breastfeeding-and-medication.co.uk/wp-content/uploads/2023/08/Moviprep-and-breastfeeding-1.pdf
An increasing number of breastfeeding mothers are having colonoscopies to investigate gut problems. The first stage of a colonoscopy is the use of a strong laxative and 24 hours of a fluid only diet to clear out the gut so that the professionals can see the gut in its entirety completely.
Many mothers worry that not eating for 24 hours will reduce their milk supply. Fasting does drop the supply a small amount for some women but frequent feeds seem to overcome problems. It is important to keep drinking the clear fluids which are allowed in order not to dehydrate.
From experience you may find that you need someone else in the house to take the baby urgently when you have to rush to the toilet – there is no waiting! You may find otherwise that you end up feeding whilst on the loo for practical reasons. The bowel washouts produce considerable urgency
Movicol®
One of the most commonly used laxative agents to clear the gut is Movicol ® otherwise known as polyethylene glycol- electrolyte solution. It is a saline laxative which is not absorbed from the gut but pulls water into the bowel to wash the contents out. Because it is not absorbed from the gut it cannot get into breastmilk and would not affect the baby.
MoviPrep®
This dual sachet product contains macrogol and electrolytes in 2 different sachets, Because it is not absorbed from the gut it cannot get into breastmilk and would not affect the baby.
Plenvu ®
This powder contains macrogol and electrolytes in sachets, Because it is not absorbed from the gut it cannot get into breastmilk and would not affect the baby.
Picolax®
Sodium picosulfate is not absorbed from the gastrointestinal tract, and its active metabolite, which is absorbed, is not detectable in breastmilk. Breastfeeding can continue as normal.
KleanPrep ®
KleanPrep contains macrogol 3350 , an osmotic laxative with a high molecular weigh and zero oral bioavailabilty. Like Moviprep it accumulates water into the GI tract, where it acts as a laxative. It would be very unlikely to enter the plasma of the mother, or milk.
Citramag®
The ingredients magnesium carbonate and citric acid will form an osmotic laxative by pulling water into the bowel and stimulating the bowel to evacuate. Poor oral absorption of magnesium make it unlikely that any will be absorbed from milk to affect the breastfed baby.
Senna
Senna is a stimulant laxative. Its key ingredient (anthraquinone), is believed to increase bowel activity due to secretion into the colon. It may produce abdominal cramps. In one study of 23 women who received Senokot none was detectable in their milk.[1] Of 15 mothers reporting loose stools, two infants had loose stools (Werthmann 1973). However, in a randomized, double-blind trial comparing Senokot tablets to placebo, of the women in the study, 126 breastfed their infants and took senna while 155 control mothers breastfed their infants. There was no difference in the percentages of infants in the active and control groups with loose stools or diarrhoea (Shelton 1980). In this study 8 doses were taken. In bowel preparation a single dose only is used.
Werthmann MW Jr, Krees SV. Quantitative excretion of Senokot in human breast milk. Med Ann Dist Columbia. 1973;42:4-5.
Shelton MG. Standardized senna in the management of constipation in the puerperium. A clinical trial. S Afr Med J. 1980;57:78-80.
Phosphate enema (Fleet®)
Sodium phosphate is a saline laxative which sucks water into the lumen of the bowel. Whilst some phosphate may get into the plasma, it is very unlikely to change the levels in milk. The oral bioavailabilty is zero to 20%. Use of phosphate enemas should not require interruption of breastfeeding (LactMed)
Bisacodyl (Dulcolax ®)
Bisacodyl is poorly absorbed from the gut (oral bioavailabilty <5%) and so reaches low levels in breastmilk. It is a stimulant laxative. Breastfeeding can continue as normal
For information on sedatives (midazolam, fentanyl, pethidine) used in colonoscopies see separate fact sheet . These also do not preclude normal breastfeeding as soon as the mother is awake and alert.
Bismuth subsalicylate (Pepto Bismol®) and Breastfeeding
Another of the frequently asked questions is the use of Pepto Bismol™ for indigestion or nausea
Pepto Bismol™ is marketed to relieve symptoms of upset stomach and diarrhoea. It’s active ingredient is bismuth subsalicylate, so it is related to aspirin which we avoid during breastfeeding at painkilling doses.
We are unsure if bismuth subsalicylate passes into a mother’s breast milk. Although bismuth salts are poorly absorbed from the maternal GI tract, significant levels of salicylate could be absorbed in theory. There are currently no reports of Reye’s syndrome in babies exposed to bismuth subsalicylate and it is normally only used very short term for stomach upset.
Breastfeeding mothers would be well advised to use alternative products to treat acute diarrhoea E.g. loperamide (Imodium®) if possible. However, In my experience of queries Pepto Bismol may be the only product available late at night and at weekends. The risk of short term use is probably low although this cannot be proved. The decision remains with the mother as to whether she wants to take it. Continuing to breastfeed during a stomach upset transfers antibodies to the baby to offer protection from the bacterial or viral condition.
It is also advertised to treat heartburn and indigestion for which there are many alternative remedies which are safe in breastfeeding, containing aluminium, calcium and magnesium carbonate.
See also https://www.e-lactancia.org/breastfeeding/bismuth-sub-oxysalicylate-2/synonym/
A very small amount of bismuth is absorbed from the gut: ≈ 0.1% (Tora 2020, Chen 2010, Boertz 2009, Dresow 1992, Nwokolo 1990: Bismuth is not absorbed into the systemic circulation of the mother, so it cannot be excreted in breast milk.
Salicylate is well absorbed (Nwokolo 1990), but is excreted in breast milk in negligible amounts, and the infant receives a relative dose of 1% (see Aspirin) and no cases of Reye’s syndrome have been reported after taking bismuth salicylate or other non-acetylated salicylate compounds.
Due to the otherwise minimum risk of Reye’s syndrome and the indiscriminate use of bismuth subsalicylate for treatment of gastroenteritis cannot be justifiable since most of gastroenteritis do not require medication instead a simply adequate hydration, a safer alternative should be desirable while breastfeeding. (Chen 2010, Nice 2000)
Ankylosing spondylitis and Breastfeeding
From my book Breastfeeding and Chronic Medical Conditions available on Amazon
“From a slightly alternative angle… I have ankylosing spondylitis, thankfully mild. I used to have quite bad pain and stiffness in the mornings and was fairly reliant on NSAIDs. Since breastfeeding (6 years continuously over 2 children now!) these symptoms are basically gone! I put it down to being pretty “active” feeding overnight so do not get a chance to stiffen up!“
“I have a chronic degenerative back condition called ankylosing spondylitis. Breastfeeding was difficult once my condition returned 3 months after birth (was in remission in pregnancy) especially when he was cluster feeding, sitting and not moving for long periods of time caused intense pain but I did what I had to give my boy the best I could. I have also had to try different medications as breastfeeding meant I could not take what I was taking before being pregnant. My little boy is now 8 months old and I could not be more proud that I am still breastfeeding“
Description
Ankylosing spondylitis is a chronic arthritic condition in which the spine and other areas of the body become inflamed. It commonly develops in teenagers and young adults. It is twice as common in men as in women. Back pain and stiffness last at least 30 minutes and then eases through the day or with activity. Commonly the pain causes night waking. Some sources describe pain in one or both buttocks and sometimes the backs of the thighs.
Symptoms include pain and swelling in other parts of the body: inflammation of the joints and where a tendon joins a bone as well as extreme fatigue.
Treatment
- Exercise and physiotherapy to improve movement.
- NSAIDs – ibuprofen, diclofenac, and naproxen all of which are compatible with breastfeeding.
- Anti TNF medication – adalimumab, Certolizumab pegol, Etanercept, Golimumab and Infliximab. These are large molecules which cannot be absorbed from breastmilk.
- Steroid tablets and injections into affected joints which are compatible with breastfeeding
- Assessment of risk of osteoporosis and treatment where necessary. See Section on Osteoporosis.
Further Information:
National Axial Spondylarthritis Society https://nass.co.uk/
Lowering / stopping milk supply and Breastfeeding
Sometimes mothers want to reduce their breastmilk supply. I’ve provided some information and links on herbs and medications – some things have evidence of effectiveness, many do not.
pdf lowering or stopping breastmilk supply
Sometimes mothers experience problems with excessive milk supply especially when weaning. Others may need or wish to stop their milk supply suddenly for a variety of reasons. Several options have been suggested;
Herbal products
- Sage can be used as the herb, as a tea or as drops which are consumed can lower supply https://kellymom.com/bf/can-i-breastfeed/herbs/herbs-oversupply/
- Jasmine flowers. In a 1998 study the use of topical application of jasmine flowers was compared to bromocriptine to suppress lactation immediately after birth. ( Shrivastav P, George K, Balasubramaniam N, Jasper MP, Thomas M, Kanagasabhapathy AS. Suppression of puerperal lactation using jasmine flowers (Jasminum sambac). Aust N Z J Obstet Gynaecol. 1988 Feb;28(1):68-71.)
Abstract (https://www.ncbi.nlm.nih.gov/pubmed/3214386?dopt=Abstract)
“The efficacy of jasmine flowers (Jasminum Sambac) applied to the breasts to suppress puerperal lactation was compared that of Bromocriptine. Effectiveness of both regimens was monitored by serum prolactin levels, clinical evaluation of the degree of breast engorgement and milk production and the analgesic intake. While both bromocriptine and jasmine flowers brought about a significant reduction in serum prolactin, the decrease was significantly greater with bromocriptine. However, clinical parameters such as breast engorgement, milk production and analgesic intake showed the 2 modes of therapy to be equally effective. The failure rates of the 2 regimens to suppress lactation were similar; however, rebound lactation occurred in a small proportion of women treated with bromocriptine. Jasmine flowers seem to be an effective and inexpensive method of suppressing puerperal lactation and can be used as an alternative in situations where cost and nonavailability restrict the use of bromocriptine.” Kellymom reports that other herbs can be used to decrease supply but no evidence from research is supplied to support the statement Peppermint, Spearmint, Parsley,
- Chickweed, Black Walnut, stinging nettles Yarrow, Herb Robert Lemon Balm, Oregano, Periwinkle Herb, Sorrel.
Normal consumption of the herbs as foodstuffs or drinking peppermint tea would not be likely to decrease supply.
Lowered milk supply as a side effect of medication
- Drugs known to lower milk production as a side effect of use as medication are the combined contraceptive pill and the decongestant pseudoephedrine. Use to deliberately lower supply is not supported by research and effects vary with individuals.
Medication to stop milk supply
Two drugs have been marketed to stop milk production. These are bromicriptine (Parlodel ®) and cabergoline (Dostinex®). In the past they have been commonly used to dry up the milk of mothers of babies born sleeping or those who die soon after birth. In this situation the mother’s body will initiate milk production as normal.
These drugs have very severe side-effects, including vomiting, postural hypotension, fatigue, dizziness and dry mouth. Also, particularly with high doses, women may suffer confusion, psychomotor excitation, hallucinations; rarely diarrhoea, gastro-intestinal bleeding, gastric ulcer, abdominal pain, tachycardia, bradycardia, arrhythmia, insomnia, psychosis, visual disturbances, and tinnitus. Cabergoline can also cause depression. They should be avoided if the mother has experienced pre-eclampsia. Both drugs can produce sudden onset sleep or excessive daytime drowsiness and driving should be avoided.
The BNF contains a warning on the use of bromocriptine:
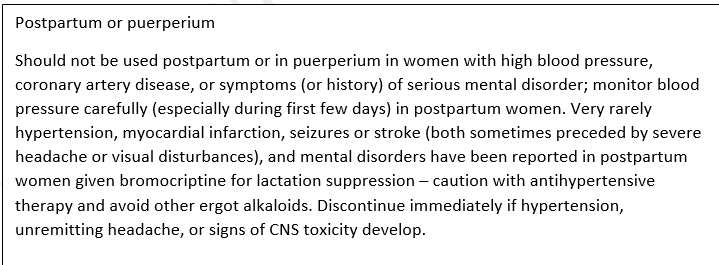
Although bromocriptine and cabergoline are licensed to suppress lactation, they are not recommended for routine suppression when women have decided not to breastfeed, or for the relief of symptoms of postpartum pain and engorgement that can be adequately treated with simple analgesics and breast support. If a dopamine-receptor agonist is required, cabergoline is preferred.
The FDA approved indication for the use of bromocriptine for lactation suppression has been withdrawn, and it is no longer approved for this purpose due to numerous maternal deaths. In 2015, the French pharmacovigilance program published a review of the adverse events associated with bromocriptine use to cease lactation. This group reported 105 serious adverse reactions including cardiovascular (70.5%), neurological (14.4%) and psychiatric (8.6%) events. There were also two fatalities: one 32-year-old female had a myocardial infarction with an arrhythmia, and a 21-year-old female had an ischemic stroke (reported in Hale online, accessed August 2016).
For the suppression of established lactation, cabergoline 0.25mg is taken every 12 hours for two days for a total of 1mg. However, this drug also has significant side effects, including headache, dizziness, fatigue or insomnia, orthostatic hypotension (feeling faint when you stand up), oedema, nose bleed, dry mouth, inhibition of lactation, nausea, constipation, anorexia and weakness. There may of course also be interactions with the drugs prescribed that have caused the cessation of breastfeeding.
For some mothers the choice to donate their breastmilk, following loss of their baby is a comfort and seen as a tribute to the baby’s memory. https://goo.gl/fxA8Xi
“In 1975, when I gave birth to my stillborn daughter, I was given a dry up shot without them even mentioning donating to milk banks as an option. There were a lot of them in those years before HIV/AIDS became an issue. I would have LOVED donating Marisa’s milk. -Chantal”
“A counselor at the hospital instructed her in techniques to dry up her milk.”
“It’s funny,” Weidner said. “No one told me about milk donation. I don’t know how I knew about it. I learned when I was planning the C-section, I knew donor milk was an option, but didn’t know who donated it, never suspected I would become one who would be a milk donor.”
Natural reduction of milk supply
In an ideal world it is better to allow the breastmilk supply to dwindle slowly, by dropping one feed at a time or expressing/feeding only when the breasts become uncomfortably full. It may however be necessary to speed up this process up, but it is still important to avoid blocked ducts and mastitis. It is possible to treat the breasts as in the early days of engorgement, using simple analgesics and cold savoy cabbage leaves in a firm but well-fitting bra. Or the mother can express just enough milk to remain comfortable frequently changing breast pads, which may become soaked as milk leaks from the breasts. Restricting the fluids which the mother is drinking will not help the milk to dry up; nor will the use of laxatives to remove water from the body.

Botox and Fillers and Breastfeeding
There is no published research that I have been able to find and trust on the passage of fillers into milk so I cant say that they are safe or unsafe. I just do not know.
There is some information from one mother who caught botulism from eating fermented salmon eggs. She continued to breastfeed. No botulinum toxin or botulism was found in the breastmilk or the baby. The doses that are used medically are far lower than that which would have caused the mother’s botulism so the amount in breastmilk is assumed to be too low to produce adverse effects.
In February 2024 a study of 4 mothers was published https://www.liebertpub.com/doi/abs/10.1089/fpsam.2023.0326
Objective: To detect the presence of botulinum toxin in breast milk from lactating subjects treated with facial botulinum toxin injections, as measured by enzyme-linked immunosorbent assay (ELISA).
Methods: For this pilot study, lactating women were injected with standardized facial botulinum toxin type A (BTXA) (range 40–92 U). Collected breast milk samples over 5 days were analyzed for the presence of botulinum toxin. Exclusion criteria included (1) lactating women still using their breast milk for their infant, (2) muscular disorders, (3) any medication that could interfere with neuromuscular function, (4) uncontrolled systemic disease, (5) pregnant, and (6) neuromodulator injection in the past 90 days.
Results: Four lactating women were recruited. Eight samples had no BTXA detected, whereas 8 of the 16 total had detectable amounts, which were well below the reported lethal oral dose for an infant.
Conclusion of the authors: Although the exclusion of lactating women from receiving cosmetic botulinum toxin injections is out of an abundance of caution to the theoretical risk to the infant, this study helps support the notion that facial botulinum toxin injections do not warrant an interruption in breastfeeding. Further studies with larger sample sizes are needed.
Caroline Hudson, Parker Wilson, David Lieberman, Harry Mittelman, and Sachin Parikh.Analysis of Breast Milk Samples in Lactating Women After Undergoing Botulinum Toxin Injections for Facial Rejuvenation: A Pilot Study.Facial Plastic Surgery & Aesthetic Medicine.ahead of print
References
1. Lee KC, Korgavkar K, Dufresne RGJ et al. Safety of cosmetic dermatologic procedures during pregnancy. Dermatol Surg. 2013;39:1573-86.
2. Middaugh J. Botulism and breast milk. N Engl J Med. 1978;298:343.
Both these cosmetic procedures have to be undertaken with this limited information in mind. It is your choice .
Vaccinations and Breastfeeding
Taken from Breastfeeding and Chronic Medical Conditions available from Amazon.
Most vaccinations can be undertaken during breastfeeding as they do not pass into breastmilk. For detailed information please check the Green Book which has sections for breastfeeding. https://www.gov.uk/government/collections/immunisation-against-infectious-disease-the-green-book
- Chicken pox (varicella): compatible with normal breastfeeding
- Hepatitis A: compatible with normal breastfeeding
- Hepatitis B: Vaccinations are routinely offered to healthcare professionals who may come into contact with body fluids. Compatible with normal breastfeeding
- Influenza: compatible with normal breastfeeding
- Meningococcal C: Immunization of pregnant or lactating women with meningococcal vaccine increased the specific secretory IgA content of milk. compatible with normal breastfeeding
- MMR Injections: A breastfeeding mother can have an MMR injection if she is not rubella immune. Although live vaccines multiply within the mother’s body, the majority have not been demonstrated to be excreted in human milk (Bohlke K, Galil K, Jackson LA, et al. Postpartum varicella vaccination: is the vaccine virus excreted in breast milk? Obstet Gynecol 2003; 102:970–7). Although rubella vaccine virus might be excreted in human milk, the virus usually does not infect the infant. If infection does occur, it is well-tolerated because the virus is attenuated. Inactivated, recombinant, subunit, polysaccharide, conjugate vaccines, and toxoids pose no risk for mothers who are breast feeding or for their infants.
- Pneumonia: compatible with normal breastfeeding
- Polio: The injectable polio vaccine is inactivated and poses no risk when given to mothers who are breastfeeding. The oral vaccine may reduce the production of antibodies by the infant and immunisation of the mother before the infant reaches 6 weeks of age is not recommended.
- Tetanus Vaccination: One study of previously vaccinated infants found that at 21 to 40 months of age breastfed infants had higher IgG levels against diphtheria, higher secretory IgA levels in saliva against diphtheria and tetanus and higher faecal IgM against tetanus than formula-fed infants. There is no contra indication to a breastfeeding mother having this vaccination.
- Tuberculin and BCG: There is no reason to avoid tuberculin testing during breastfeeding nor to avoid use of the BCG vaccine unless the mother is immunocompromised.
- Typhoid Vaccination: One study of previously vaccinated infants found that at 21 to 40 months of age breastfed infants had higher IgG levels against diphtheria, higher secretory IgA levels in saliva against diphtheria and tetanus and higher faecal IgM against tetanus than formula-fed infants. There is no contra indication to having the vaccination and continuing to breastfeed.
- Whooping Cough: there is no evidence of risk of vaccinating breastfeeding mothers with the whooping cough (pertussis) vaccine as part of the campaign to protect new-born babies.
See also SPS Giving vaccines and breastfeeding
https://www.sps.nhs.uk/articles/giving-vaccines-during-breastfeeding/
Dihydrocodeine and breastfeeding
I keep being asked about strong analgesics in breastfeeding. Lots of people seem unaware that codeine and dihydrocodeine sound similar but do not have the same risk in breastfeeding. Although many babies dont exhibit drowsiness when exposed to codeine during breastfeeding, dihydrocodeine is preferred.
This explains why:
The analgesic effect of dihydrocodeine appears to be mainly due to the parent compound. The oral bio availability of dihydrocodeine is 20% due to substantial first pass metabolism. The half life is quoted as 3.5-5h . It is metabolised in the liver by CYP2D6 to dihydromorphine, which has potent analgesic activity. However, the CYP2D6 pathway only represents a minor route of metabolism, with other metabolic pathways being involved.
The metabolism of dihydrocodeine is not affected by individual metabolic capacity as the analgesic effect is produced by the parent drug compared to codeine which is a pro drug.
Dihydrocodeine may be the preferred weak opioid for postoperative use in the breastfeeding woman, because of its cleaner metabolism compared with codeine and wide experience of use after caesarean section. As with any strong painkillers the baby should be monitored for drowsiness and changes in feeding pattern. Dihydrocodeine may be combined with paracetamol as co-dydramol.
All opioids can cause nausea and dizziness but almost invariably cause constipation so it is wise to commence stool softeners like lactulose and/or docusate both of which are compatible with breastfeeding as they don’t pass into milk.
See https://breastfeeding-and-medication.co.uk/fact-sheet/constipation-laxatives-and-breastfeeding
Midazolam as a sedative for procedures in breastfeeding mothers
The reason I write these factsheets is in response to the questions which are posed to me on social media. I have included the use of midazolam in fact sheets on colonoscopy, endoscopy and dental sedation on information on the Breastfeeding Network but still mothers are told that they need to delay procedures, are only allowed gas and air during the procedure or must stop breastfeeding for 24 hours. The latter is recommended by the manufacturers but since the half life is 3 hours it is all gone from the mother’s body and therefore her milk within 15 hours. However, looking at the pharmacokinetics of midazolam use as a single dose sedative is not a contra indication to normal breastfeeding as confirmed
Guideline on anaesthesia and sedation in breastfeeding:
https://associationofanaesthetists-ublications.onlinelibrary.wiley.com/doi/full/10.1111/anae.15179
“Midazolam: extensive first-pass metabolism results in low systemic bioavailability after oral doses, so blood levels in the infant after breastfeeding can be expected to be low [20]. Breastfeeding can be resumed after a single dose of midazolam as soon as the woman has recovered from the procedure.”
Midazolam and endoscopy factsheet
This factsheet contains information taken from my book Breastfeeding and Medication 2018. I hope it helps breastfeeding mums and professionals