Home » Articles posted by Wendy Jones
Author Archives: Wendy Jones
Inflammatory Bowel Disease (IBD) and Pregnancy
I have written quite a lot about IBD and breastfeeding and compiled information on medication and tests https://breastfeeding-and-medication.co.uk/wp-content/uploads/2022/04/IBD-and-breastfeeding-factsheet-June-2021.pdf. The use of medication in pregnancy is not my area of expertise and I am purely providing links to those who know more.
This information is taken from The medicines Use in Pregnancy Site BUMPS https://www.medicinesinpregnancy.org/About-Us/ and is presented here for ease of access for parents and professionals.
Health professionals can consult the team https://uktis.org/contact-us/ but not members of the public.
Further information is also available https://crohnsandcolitis.org.uk/info-support/information-about-crohns-and-colitis/all-information-about-crohns-and-colitis/living-with-crohns-or-colitis/pregnancy-and-breastfeeding
Links to information on medication
Do not stop taking medication without discussing with your GP or IBD team
For many of the medications used to control symptoms of IBD in pregnancy live vaccines (rotavirus and if necessary BCG) should not be given to a baby under 6 months. If rotavirus is given to the baby then the mother should wear gloves during nappy changes for 2 weeks to avoid exposure to live viral fragments shed in faeces. https://breastfeeding-and-medication.co.uk/fact-sheet/live-vaccinations-and-immunosuppressant-medication-taken-by-breastfeeding-mothers
Prednisolone https://www.medicinesinpregnancy.org/leaflets-a-z/prednisolone/
What are the benefits of using a systemic corticosteroid in pregnancy?
Corticosteroids reduce inflammation by stopping the immune system from attacking the body’s tissues. This is important to reduce unpleasant symptoms and prevent long-term damage. It may also lower the chance of some pregnancy problems linked to uncontrolled inflammation, including miscarriage and lower birth weight.
Are there any risks of using a systemic corticosteroid in pregnancy?
Corticosteroid use in early pregnancy has been linked in some (but not all) studies to a higher chance of having a baby with a cleft lip and/or palate. However, it is clear that the vast majority of babies exposed in the womb to systemic corticosteroids are born without these conditions.
Women taking a systemic corticosteroid in pregnancy may have a higher chance of having a preterm birth. However, it is thought likely that at least some of this effect is due to the underlying inflammatory conditions in these women which have themselves been linked to preterm birth.
Are there any alternatives to using a systemic corticosteroid in pregnancy?
Possibly. Other medicines can often be used to treat inflammatory conditions during pregnancy. However, systemic corticosteroids are usually considered to be among the safest options and are often recommended as a first-choice medicine to treat rheumatic and auto-immune disease during pregnancy.
Some women may find that their symptoms improve during pregnancy; if so, their specialist may advise that their medicine(s) can be altered. However, women should not change or stop their medication without speaking to their doctor.
Azathioprine https://www.medicinesinpregnancy.org/leaflets-a-z/azathioprine/
What are the benefits of using azathioprine/mercaptopurine in pregnancy?
Azathioprine and mercaptopurine reduce inflammation by stopping the immune system from attacking the body’s tissues. This is important to reduce unpleasant symptoms and prevent long-term damage. It may also lower the chance of some pregnancy problems linked to uncontrolled inflammation, including miscarriage and lower birth weight. It is also vital for both mother and baby that a transplanted organ continues to function well during pregnancy.
What are the risks of using azathioprine/mercaptopurine in pregnancy?:
There is no evidence that use of azathioprine or mercaptopurine harm the baby if taken in pregnancy.
Sulfasalazine https://www.medicinesinpregnancy.org/leaflets-a-z/sulfasalazine/
What are the benefits of taking sulfasalazine in pregnancy?
Sulfasalazine reduces ongoing tissue damage caused by ulcerative colitis, Crohn’s disease, and rheumatoid arthritis. It also controls unpleasant symptoms that can affect quality of life, and can help to prevent the pregnancy complications that have been associated with these illnesses.
Are there any risks of taking sulfasalazine during pregnancy?
There are no concerns that taking sulfasalazine in pregnancy causes problems in the baby and it is routinely prescribed for pregnant women with ulcerative colitis, Crohn’s disease, and rheumatoid arthritis.
Because sulfasalazine can potentially affect folic acid levels, women taking it while trying to conceive and during pregnancy should be prescribed a high dose folic acid supplement.
Infliximab https://www.medicinesinpregnancy.org/leaflets-a-z/infliximab/
What are the benefits of using infliximab in pregnancy?
Infliximab helps to stop the immune system from attacking the body. It controls the unpleasant and often disabling symptoms of some autoimmune diseases and helps to prevent ongoing damage to tissues and organs.
What are the risks of using infliximab in pregnancy?
The available data suggests that infliximab is unlikely to affect the baby’s development. There are reports of some babies being born with a low infant birth weight following infliximab exposure. However, it is unclear if this is caused by the drug itself or the underlying illnesses in pregnant women taking infliximab.
Certolizumab https://www.medicinesinpregnancy.org/leaflets-a-z/certolizumab/
What are the benefits of using certolizumab in pregnancy?
Certolizumab reduces inflammation by stopping the immune system from attacking the body’s tissues. This is important to reduce unpleasant symptoms and prevent long-term damage. It may also lower the chance of some pregnancy problems linked to uncontrolled inflammation, including miscarriage and lower infant birth weight. Certolizumab does not easily cross the placenta so only tiny amounts reach the baby. It is therefore not expected to cause problems in pregnancy.
What are the risks of using certolizumab in pregnancy?
There are no known risks. Use of certolizumab has been studied in around 1,400 pregnant women and there is no evidence that it affects the baby’s development.
Adalimumab https://www.medicinesinpregnancy.org/leaflets-a-z/adalimumab/
What are the benefits of using adalimumab in pregnancy?
Adalimumab reduces inflammation by stopping the immune system from attacking the body’s tissues. This is important to reduce unpleasant symptoms and prevent long-term damage. It may also lower the chance of some pregnancy problems linked to uncontrolled inflammation, including miscarriage and lower infant birth weight.
What are the risks of using adalimumab in pregnancy?
Use of adalimumab in pregnancy has been studied in around 1,500 women. There is no suggestion that adalimumab affects the baby’s development, but ongoing data collection is ideally required to confirm this.
Etanercept https://www.medicinesinpregnancy.org/leaflets-a-z/etanercept/
What are the benefits of using etanercept in pregnancy?
Etanercept reduces inflammation by stopping the immune system from attacking the body’s tissues. This is important to reduce unpleasant symptoms and prevent long-term damage. It may also lower the chance of some pregnancy problems linked to uncontrolled inflammation, including miscarriage and lower infant birth weight.
What are the risks of using etanercept in pregnancy?
Use of etanercept in pregnancy has been studied in around 1,200 women. There is no suggestion that etanercept affects the baby’s development but ongoing data collection is ideally required to confirm this.
Ustekinumab https://www.medicinesinpregnancy.org/leaflets-a-z/ustekinumab/
What are the benefits of using ustekinumab in pregnancy?
Ustekinumab helps to stop the immune system from attacking the body. It controls the unpleasant and often disabling symptoms of some autoimmune diseases, and helps to prevent ongoing damage to tissues and organs. It can also reduce the risk of some adverse pregnancy outcomes that have been linked to poorly controlled autoimmune disease, including miscarriage, preterm delivery and low infant birth weight.
Are there any risks of using ustekinumab during pregnancy?
The small amount of data available suggests that ustekinumab is unlikely to harm the baby but further studies are ideally required.
Quetiapine and breastfeeding
One of the questions that comes up frequently. Often mothers told that they cannot breastfeeding if they need quetiapine for their own menatl health
Hope this information helps them make an infomed decision
PDF of factsheet available here
https://breastfeeding-and-medication.co.uk/wp-content/uploads/2022/06/quetiapine.pdf
The information on this sheet is based upon my professional experience as a pharmacist with a specialised interest in the safety of drugs in breastmilk, supported by evidence from expert sources. However, I cannot take responsibility for the prescription of medication which remains with the healthcare professionals involved. I am happy to discuss the evidence by email wendy@breastfeeding-and-medication.co.uk
Quetiapine is probably compatible with use during breastfeeding in dose less than 400mg daily based on limited studies and low theoretical infant dose. Be aware of possibility of drowsiness in the baby. Mother should not fall asleep with the baby in bed, on a settee or chair.
Bipolar disease description
Bipolar disorder is a mental health condition that affects moods. The latter can swing from one extreme of lethargy and depression to a feeling of being high and overactive hence the original name of manic depression. During bouts of depression, it is not uncommon to feel suicidal or worthless and it is important to recognise this and seek a place of safety or a person you trust as quickly as possible. During a manic phase there may be feelings of having lots of energy, ambitious plans and idea. It is not uncommon to spend large amounts of money on expensive, unwanted goods and some people ask their banks to block spending above a certain level to avoid debt. It is also common to not feel like eating or sleeping, to talk quickly and become easily annoyed. For some this phase is a positive experience and a time of creativity so may reject medication. It may also become a psychotic phase where things which do not exist may be seen and heard (voices controlling actions). It is a complex condition which may need adjustments. Around one in every 100 people will be diagnosed with it at some point in their life. It frequently develops between 15 and 19 years of age but rarely after 40. The incidence is the same in men and women. The pattern of mood swings in bipolar disorder varies widely. Some people only have a couple of episodes in their lifetime and are stable in between, while others have many episodes. Diagnosis is made only after one episode of mania as well as the depression. In this state the mother may have an elated mood or alternatively she may feel irritable and angry. She may experience racing thoughts rapidly changing from one area to another. It may be impossible for her to be still, but the activity may be unproductive. It is reported to affect a higher proportion of intelligent people with gifted creativity.
Quetiapine (Seroquel™)
Quetiapine is an Atypical anti-psychotic. Quetiapine may also be used in severe depression. In general, atypicals may be better tolerated with fewer extra-pyramidal side effects than the older drugs e.g., chlorpromazine and haloperidol . However, they do produce weight gain and a risk of hyperglycaemia which may need to be monitored regularly. Quetiapine has been associated with a low incidence of extra-pyramidal symptoms, but tardive dyskinesia may occur after long-term treatment. The most frequent adverse effects with quetiapine are somnolence and dizziness. Weight gain, particularly during early treatment, has also been noted. It appears to have a minimal effect on prolactin levels Lee et al. (2004) studied one mother taking 200 mg daily throughout pregnancy. Breastfeeding was not initiated in the absence of safety data until measurement of her breastmilk samples were available. Levels measured indicated that an exclusively breastfed baby would normally ingest only 0.09% of the weight adjusted dose (maximum 0.43%). The mother initiated breastfeeding 8 weeks after delivery. Follow up at 4.5 months indicated normal development with no adverse effects. Misri et al. (2006) studied six mothers taking 25 to 400 mg daily together with an antidepressant. In mothers taking less than 75 mg, milk levels were below the level of detection. One mother taking 400 mg daily had a level of drug in her milk of 101 µg per litre. Mental and psychomotor tests were below the norm in two of the infants when monitored up to 18 months of age although within the norm. The authors concluded this result was due to effects other than exposure to the drug. Several other case study reports of quetiapine use have been reported with low levels of drug reported in the babies and no adverse reactions directly attributable to the drug identified (Rampono et al. 2007; Kruninger et al. 2007; Balke 2001; Seppala 2004; Ritz 2005; Gentile 2006). A relative infant dose quoted as 0.070.1% is quoted (Hale online access).
Summary of Use during Lactation (LactMed https://www.ncbi.nlm.nih.gov/books/NBK501087/
Maternal quetiapine doses of up to 400 mg daily produce doses in milk that are less than 1% of the maternal weight-adjusted dosage. Limited long-term follow-up of infants exposed to quetiapine indicates that infants generally developed normally. A safety scoring system finds quetiapine to be possible to use during breastfeeding.[1] Systematic reviews of second-generation antipsychotics concluded that quetiapine seemed to be the first- or second-choice agent during breastfeeding.[2-4] Monitor the infant for drowsiness and developmental milestones, especially if other antipsychotics are used concurrently. E Elactancia https://www.e-lactancia.org/breastfeeding/quetiapine-fumarate/product/ Quetiapine is excreted into breast milk in clinically insignificant amounts. (Yazdani 2018, Aydin 2015, Van Boekholt 2015, Rampono 2007, Misri 2006, Lee 2004, Seppala 2004). Clinical or development problems in infants whose mothers were treated have not been observed, whether at the short or long term. (Levesque 2016, Sharma 2016, Aydin 2015, Van Boekholt 2015, Newport 2009, Rampono 2007, Misri 2006, Ritz 2005, Gentile 2005, Seppala 2004, Lee 2004). Very low plasma-levels of quetiapine in these infants were found. (Rampono 2007). Galactorrhoea may occur with or without an increase of prolactin. (Glocker 2021, Suttajit 2013, Mushtaq 2012, Sethi 2010, Gupta 2007, Atmaca 2002). Expert authors consider the use of quetiapine to be safe or very probably safe during breastfeeding. (Hale, Lactmed, Uguz 2021, Teodorescu 2020, Rybakowski 2019, Pacchiarotti 2016, Schaefer 2015, Grover 2005, Larsen 2015, Parikh 2014, Rowe 2013) Pharmacokinetics (Hale) Quetiapine is 83% plasma protein bound. The half-life is 6 to 7 hours. Milk plasma ratio 0.3. Relative infant dose 0.02% – 0.1% Other a typical drug options • risperidone (Risperidal™): Limited information indicates that maternal risperidone doses of up to 6 mg daily produce low levels in milk. Observe baby for drowsiness but no adverse events reported to date. • olanzapine (Zyprexa™): Maternal doses of olanzapine up to 20 mg daily produce low levels in milk and undetectable levels in the serum of breastfed infants. Monitor the baby for drowsiness and effective feeding. • aripiprazole (Ablify ™): Limited information indicates that maternal doses of aripiprazole up to 15 mg daily produce low levels in milk. However, it inhibits prolactin levels and despite expert advice it may not be possible to achieve a full milk supply ((Mendhekar 2006, Nordeng 2014). References
• Balke LD, Quetiapine effective in the treatment of bipolar affective disorder during pregnancy, World J Biol Psychiatry, 2001;2:303S. Abstract P02115.
• Drugs and Lactation Database (LactMed) https://www.ncbi.nlm.nih.gov/books/NBK501922/ • E Elactancia https://www.e-lactancia.org/
• Gentile S, Quetiapine-fluvoxamine combination during pregnancy and while breastfeeding, Arch Women’s Ment Health, 2006;9:158–9.
• Hale TW Medications and Mothers Milk online access Springer Publishing
• Jones W Breastfeeding and Medication Routledge 2018 • Jones W Breastfeeding and Chronic Medical Conditions Amazon 2020
• Kruninger U, Meltzer V, Hiemke C et al. [Pregnancy and lactation under treatment with quetiapine Psychiatr Prax Suppl, 2007;34:S756.
• LactMed
• Lee A, Giesbrecht E, Dunn E, Ito S, Excretion of quetiapine in breastmilk, Am J Psychiatry, 2004;161:17156.
• Misri S, Corral M, Wardrop AA, Kendrick K. Quetiapine augmentation in lactation: a series of case reports. J Clin Psychopharmacol. 2006;26:508-11.
• Pacchiarotti I, Leon-Caballero J, Murru A et al. Mood stabilizers and antipsychotics during breastfeeding: Focus on bipolar disorder. Eur Neuropsychopharmacol. 2016;26:1562-78
• Rampono J, Kristensen JH, Ilett KF, Hackett LP, Kohan R, Quetiapine and breastfeeding, Ann Pharmacother, 2007;41:7114.
• Ritz S, Quetiapine monotherapy in post-partum onset bipolar disorder with a mixed affective state, Eur Neuropsychopharmacol, 2005;15 (Suppl. 3):S407. Abstract.
• Seppala J, Quetiapine (‘Seroquel’) is effective and well tolerated in the treatment of psychotic depression during breastfeeding, Int J Neuropsychopharmacol, 2004;7 (Suppl. 1):S245. Abstract P01.431.
Specialist Pharmacy Service Safety in Lactation: Antipsychotics 2020
E Lactancia Quetiapine : https://www.e-lactancia.org/breastfeeding/quetiapine-fumarate/product/ : Very low risk

Fluoxetine and Breastfeeding
In the final of the sheets on antidepressant / anti anxiety SSRIs is fluoxetine. It is often looked on as the least compatible with breastfeeding because of its long half life and greater passage into milk. However, it is often used in pregnancy because there are a significant number of studies https://www.medicinesinpregnancy.org/leaflets-a-z/fluoxetine/
What is perhaps less well known is that if a mother has taken it throughout pregnancy the baby MAY be very drowsy in the first few days after delivery as it withdraws from the higher levels achieved through placental transfer.
My recommendation for any mother taking fluoxetine during pregnancy and wishing to breastfeed is to learn hand expression in preparation
and to maybe discuss antenatal expression of colostrum with the midwife, just in case the baby is sleepy and taking time to latch effectively. Colostrum can raise blood sugars in very small amounts. (This is really helpful info for the red flags of low sugar and in my opinion explains everything well https://www.guysandstthomas.nhs.uk/resources/patient-information/maternity/protecting-your-baby-from-low-blood-glucose.pdf)
So you can breastfeed after delivery if you have taken fluoxetine but you may need a little help and support. Seek this antenatally so you are well prepared.
I would also add that if fluoxetine has been the SSRI that you have used and found effective in the past, then that would make it the first choice in breastfeeding. Some babies are colicky, some are drowsy, some vomit, some have loose diarrhoea – but we cant tell in advance.
I remember the very first study I looked at on fluoxetine some 25 or more years ago that the mother and the baby’s paediatrician thought the baby hadnt changed behaviour when exposed to fluoxetine via his mother’s breastmilk. The baby’s father (also a paediatrician) perceived it as more irritable and on that anecdotal basis back then it was said that fluoxetine made babies irritable. I cant find the report any more but if we had been able to see into the family unit we may have seen a dad trying to help his partner whilst working and feeling stressed himself. Who knows?
I hope this information is useful to anyone taking fluoxetine whilst breastfeeding
Fluoxetine and breastfeeding factsheet




Anxiety and breastfeeding – need to take a drug to relieve symptoms
I was very proud to have co written a fact sheet for BfN on anxiety and breastfeeding which affects so many new mothers, with my daughter. Beth is a CBT therapist and approached the treatment with non pharmacological methods available via IAPT and IESO (although with a waiting list sadly for most).
I looked at the relief of symptoms with long-term treatments such as SSRI drugs e.g. sertraline, citalopram, fluoxetine and paroxetine. Mothers may also be helped with propranolol to relieve palpitations and racing heart.
Recently there have been more requests from mothers with anxiety or post traumatic stress to take benzodiazepine to reduce symptoms or to treat a panic attack. Occasional use might be acceptable with monitoring of the baby for drowsiness and effective feeding. However, regular use is not encouraged – particularly of diazepam – because of its long half life and potential to accumulate in breastmilk and the baby, but also because this family of drugs is addictive with as little as 28 days treatment.
I have written this factsheet to provide as much information as possible on the use of anxiolytics diazepam, loprazolam and alparazolam during breastfeeding.
anxiolytics and breastfeeding factsheet
The information is taken from Breastfeeding and Medication which includes full references . Please consider buying the book if this information is useful
Anxiolytics can be used to relive anxiety disorders. Management of anxiety is best achieved by non-pharmacological methods such as counselling and cognitive behavioural therapy. Anxiolytics are not as useful to treat acute panic attacks which will dissipate naturally before the drug is absorbed.
Use of anxiolytics in lactating women is generally discouraged due to the possibility of sedation of the infant and consequential reduction in feeding efficacy and limited weight gain
Anti-depressants are used for generalised anxiety disorders, particularly selective serotonin re-uptake inhibitors (SSRIs). Beta blockers such as propranolol may also be beneficial if symptoms of palpitations predominate.
Diazepam ( Valium®)
Diazepam has a long half-life of 43 hours (with terminal metabolite being present for 2 to 5 days) and accumulation is possible with repeated doses. The plasma elimination is further extended in neonates due to poor hepatic function. A shorter-acting anxiolytic is preferable for use particularly in neonates.
Brandt (1976) conducted a study of four post-natal women who were given 10 mg diazepam at bedtime for six nights. He concluded that even with a neonate, a maternal dose of 10 mg produced breastmilk levels too small to cause any untoward effects in the baby. Erkkola and Kanto (1972) studied three infants whose mothers were taking 10 mg diazepam three times daily from delivery. The babies were observed for 6 days during which period no symptoms of sedation were noticed. However, Patrick et al. (1972) reported on a single mother taking the same dose. At 8 days of age (three days after the mother commenced diazepam) symptoms of lethargy, EEG changes and weight loss were apparent in the infant and attributed to the diazepam exposure. Relative infant dose quoted as 7.1% (Hale 2017 online access). It is licensed for use in children only to control convulsions.
Diazepam is also a drug which may be abused in large doses. It is also possible to become addicted with daily doses over just one month.
The BNF suggests that benzodiazepines are present in milk, and should be avoided if possible during breastfeeding.
Single doses of diazepam may also be used in situations such as fear of flying, before surgery or other anxiety provoking situations with continued breastfeeding as normal.
Avoid if possible. Use for a short a time as possible. Observe baby for drowsiness. Avoid falling asleep with the baby in bed on a settee or chair.
Lorazepam (Ativan®)
Lorazepam is 85% bound to plasma proteins and is 90% bio-available. Half-life is reported as 10 to 20 hours. A post-partum study (Summerfield and Nielsen 1985) found clinically insignificant amounts of lorazepam in breastmilk even at a dose of 2.5 mg twice daily for the first 5 days post-natally. Whitelaw et al. (1981) estimated that an exclusively breastfed infant would be exposed to 7 µg per kilogramme per day with a maternal dose of 2.5 mg twice daily The single infant studied showed no signs of sedation. The dose used is in this study is more than the usual maximum of 2 mg daily. Relative infant is dose quoted as 2.5% (Hale 2017 online access). It is licensed for use in children only to control convulsions.
The BNF suggests that benzodiazepines are present in milk, and should be avoided if possible during breastfeeding.
LactMed reports that : Lorazepam has low levels in breastmilk, a short half-life relative to many other benzodiazepines, and is safely administered directly to infants. Evidence from nursing mothers indicates that lorazepam does not cause any adverse effects in breastfed infants with usual maternal dosages and that no special precautions are required.
Using Kelly (2012) data lorazepam may be taken as one of the safer benzodiazepines if use is essential.
Avoid if possible. Use for a short a time as possible. Observe baby for drowsiness. Avoid falling asleep with the baby in bed on a settee or chair. May be preferable to diazepam as it has a shorter half-life and no active metabolites.
Alprazolam (Xanax®)
Alprazolam is a benzodiazepine but preferred due to the shorter half life (12-15 hours). Oo obtained multiple milk and serum samples from eight lactating subjects up to 36 hours after a single oral
doses of 0.5 mg alprazolam. The milk plasma ratio was determined to be 0.36 a level too low to produce clinically significant levels. No outcomes were available as the infants were not breastfed. Reports of withdrawal in infants exposed in utero and breastfed are documented (Anderson 1989).
The BNF states that all benzodiazepines are present in milk, and should be avoided if possible during breast-feeding.
Avoid if possible. Use for a short a time as possible. Observe baby for drowsiness. Avoid falling asleep with the baby in bed on a settee or chair. May be preferable to diazepam as it has a shorter half-life

Pain relief when breastfeeding
It is not acceptable to leave any mother in pain because she is breastfeeding nor to suggest that she could have more effective pain relief if she stopped breastfeeding.
I’m often asked about the safety of opioids during breastfeeding so this is a really interesting study
Despite opioids being used first line in emergency settings to treat severe acute extremity pain, there is limited evidence available to inform this practice.
In a study in JAMA (7 November 2017), researchers randomly assigned 416 patients in the emergency department with moderate-to-severe acute extremity pain to one of the following groups: 400mg ibuprofen/1000mg paracetamol; 5mg oxycodone/325mg paracetamol; 5mg hydrocodone/300mg paracetamol; or 30mg codeine/300mg paracetamol[1].
https://jamanetwork.com/journals/jama/article-abstract/2661581?redirect=true
I have written this powerpoint presentation which I hope explains the analgesic ladder and helps professionals to understand the compatibility of analgesics and breastfeeding
- Paracetamol or NSAID
- Paracetamol + NSAID
-
Paracetamol+NSAID+Opioid (at the lowest possible dose for the shortest possible time co prescribed with a laxative)
Non steroidal anti inflammatory drugs
- Compatible with breastfeeding: ibuprofen, diclofenac (Voltarol ™, Difene™), naproxen (Naprosyn™) https://breastfeeding-and-medication.co.uk/fact-sheet/naproxen-and-breastfeeding
- No data on compatibility with breastfeeding: etoricoxin (Arcoxia™), meloxicam (Mobic™)
- See https://www.sps.nhs.uk/articles/using-nsaids-during-breastfeeding
Opioids
- compatible with breastfeeding: oral morphine, dihydrocodeine
- https://breastfeeding-and-medication.co.uk/fact-sheet/dihydrocodeine-and-breastfeeding
- use with caution as may cause drowsiness: oxycodone (Oxycontin™, Oxyfast™)
- avoid if possible as may cause drowsiness: codeine
https://breastfeeding-and-medication.co.uk/thoughts/breastfeeding-and-codeine
https://breastfeeding-and-medication.co.uk/fact-sheet/accidental-dose-of-codeine-when-breastfeeding
All opioids can cause nausea and dizziness but almost invariably cause constipation so it is wise to commence stool softeners like lactulose and/or docusate both of which are compatible with breastfeeding as they don’t pass into milk.
See
https://breastfeeding-and-medication.co.uk/fact-sheet/constipation-laxatives-and-breastfeeding
Analgesics and breastfeeding Powerpoint


see also https://www.breastfeedingnetwork.org.uk/factsheet/analgesics/
https://breastfeeding-and-medication.co.uk/fact-sheet/dihydrocodeine-and-breastfeeding
https://breastfeeding-and-medication.co.uk/thoughts/breastfeeding-and-codeine
https://breastfeeding-and-medication.co.uk/fact-sheet/migraine-treatment-and-breastfeeding
Rivaroxaban and other anticoagulants and breastfeeding
For many years the standard anti coagulants to treat and prevent deep vein thrombosis (DVT) have been heparin and low molecular weight heparionoids e.g Enoxaparin (Clexane®) or alternately but generally less frequently Tinzaparin (Innohep®), Dalteparin (Fragmin®, Fondaparinux (Arixtra®). Alternatively warfarin may be given as a tablet but generally takes too long to stabilise the clotting mechanism. All of these drugs are compatible with breastfeeding. The sub cutaneous injections are too large molecules which cannot be absorbed from breastmilk (are not orally bio-available). Because of the very low milk levels with warfarin doses less than 12 mg daily, amounts ingested by the infant are small. No adverse reactions in breastfed infants have been reported from maternal warfarin use during lactation, even with a dose of 25 mg daily for 7 days. There is a consensus that maternal warfarin therapy during breastfeeding poses little risk to the breastfed infant. No special precautions are necessary. (Lactmed https://www.ncbi.nlm.nih.gov/books/NBK501137/).
See also Using heparins during breastfeeding Jan 2024 https://www.sps.nhs.uk/articles/using-heparins-during-breastfeeding/
Although these drugs are not absorbed from milk, caution is recommended where there is donation to a milk bank of surplus breastmilk. Should any small amount reach a pre-term baby it may result in a bleed with catastrophic results. There are no studies to confirm this but the recommendation is made to protect these most vulnerable babies.
Deep vein thrombosis
Whilst DVTs are uncommon they are 5 times more common in pregnancy and in the first 6 weeks after delivery than in women who are not pregnant.
The risk of developing DVT during pregnancy is even greater if :
- there is a history or family history of DVT
- age over 35
- obese BMI >30
- a severe infection or recent serious injury, which restrict exercise
- thrombophilia
- multiple birth
- after fertility treatment
- after a caesarean section
- currently smoke
- have severe varicose veins
- dehydration
https://www.nhs.uk/pregnancy/related-conditions/complications/deep-vein-thrombosis/
If the clot breaks off into the bloodstream, it can block a blood vessel in the lungs. This is called a pulmonary embolism (PE) and needs emergency treatment. It may be investigated by a VQ or CT scan (preferably the latter as it involves no interruption of breastfeeding . See https://breastfeeding-and-medication.co.uk/fact-sheet/breastfeeding-after-vq-scans
The newer treatments to prevent clots are called Direct Oral Anticoagulant Medications (DOAC) which have advantages in that they are oral medications and need less frequent blood tests to confirm the INR.
UKDILAS have produced an excellent summary https://www.sps.nhs.uk/articles/using-oral-anticoagulants-in-breastfeeding-women/
Rivaroxaban (Xarelto®): compatible with breastfeeding
- Doses from breastmilk are over 100 times lower than doses given directly to pediatric patients. (Hale).
- Several case reports consistently indicate that maternal doses of rivaroxaban of 15 to 30 mg daily produce low levels in milk that are considerably below doses required for anticoagulation in infants (Lactmed https://www.ncbi.nlm.nih.gov/books/NBK500742/.
- Its pharmacokinetic data (large volume of distribution and high percentage of protein binding) explain the very small passage to milk observed in four different cases (Zhao 2020, Muysson 2019, Saito 2019, Wiesen 2016). https://www.e-lactancia.org/breastfeeding/rivaroxaban/product/
- See also Potential treatment option of rivaroxaban for breastfeeding women: A case series 2024. https://www.sciencedirect.com/science/article/abs/pii/S0049384824001166
- This is one of the preferred choice DOACs. Milk levels are low. Although rivaroxaban has a high oral bioavailability, very low levels are expected in milk due to its other pharmacokinetic properties, so infant exposure should still be minimal. https://www.sps.nhs.uk/articles/using-oral-anticoagulants-during-breastfeeding/
Dabigatran (Pradaxa ®) compatible with breastfeeding
- There are no studies on the transfer of dabigatran to breast milk. The molecular weight is large (628 Daltons) and the oral bioavailability is low (6.5%); therefore, clinically relevant levels are not expected to occur in a breastfed infant. (Hale).
- In adults, less than 7% of dabigatran is absorbed orally in its prodrug form of dabigatran etexilate mesylate; dabigatran itself is not absorbed orally. Preliminary data from 2 individuals indicate that dabigatran is poorly excreted into breastmilk and unlikely to affect the breastfed infant. If the mother requires dabigatran, it is not a reason to discontinue breastfeeding. Because data are limited, monitor preterm or newborn infants for signs of bleeding. (Lactmed https://www.ncbi.nlm.nih.gov/books/NBK500744/
- Its low oral bioavailability (EMA 2018, Blech 2008) hinders transfer to infant plasma via breastmilk, except in premature infants and the immediate neonatal period when there may be increased intestinal permeability.It is the oral anticoagulant with the lowest excretion in breast milk (Daei 2021). https://www.e-lactancia.org/breastfeeding/dabigatran-etexilate/product/
- This is one of the preferred choice DOACs. Milk levels are likely to be low. Dabigatran etexilate is one of the largest of the DOAC molecules and has a large volume of distribution, therefore it would be expected to pass into breast milk in low amounts. Milk levels were tested from two breastfeeding women who took dabigatran etexilate 220mg as a single dose. The relative infant dose was calculated to be between 0.01 and 0.07%. The infants did not receive any breast milk during this time. Infant absorption is likely to be low. Dabigatran etexilate also has very low oral bioavailability, so the infant is unlikely to absorb clinically significant amounts from the breast milk. It is therefore very unlikely that the infant would get any side-effects.https://www.sps.nhs.uk/articles/using-oral-anticoagulants-during-breastfeeding/
Apixaban(Eliquis®) and Edoxaban (Lixiana®) due to limited research should not be prescribed during breastfeeding.

Glucosamine and chondroitin supplements during breastfeeding
More breastfeeding mums seem to have taken up running again or for the first time. We have all needed to take exercise in this strange world the past few years.
This is the information on glucosamine and chondroitin during breastfeeding – enjoy your running. Yes it is safe in breastfeeding :
https://kellymom.com/bf/can-i-breastfeed/lifestyle/mom-exercise/
Glucosamine
Glucosamine is either derived from shellfish or synthetically produced. The shellfish derived product should be avoided by anyone with a shellfish allergy.
It is most commonly used to treat osteoarthritis and joint pain or to prevent joint damage. A glucosamine derivative, N-acetylglucosamine, is a normal component of human breastmilk. Glucosamine occasionally causes stomach discomfort in adults but is generally well tolerated. There are no studies on levels in breastmilk but it is poorly absorbed and metabolised in the liver so levels absorbed by the breastfed baby are likely to be very low.
Chondroitin
Chondroitin is a mixture of large glycosaminoglycans and disaccharide polymers, usually derived from shark or bovine cartilage. It is most commonly used to treat osteoarthritis because it acts as a flexible connecting material between the protein filaments in cartilage.
Chondroitin is poorly absorbed orally with a bioavailability of about 10%. Its molecular weight averages 50,000 Daltons so is unlikely to be absorbed by breastfed babies at all.
It is well tolerated in mothers with occasional gastrointestinal upset reported. Although no studies exist on the use of chondroitin sulphate supplements during breastfeeding, small amounts occur naturally in breastmilk. Mothers of preterm infants excrete greater amounts of chondroitin into breastmilk than mothers of fullterm infants.The use of chondroitin by a nursing mother is unlikely to adversely affect the breastfed infant.
References
Coppa GV, Gabrielli O, Zampini L et al. Glycosaminoglycan content in term and preterm milk during the first month of lactation. Neonatology. 2011;101:74-76. https://pubmed.ncbi.nlm.nih.gov/21934331/
Hale TW Medications and Mothers Milk
LactMed https://www.ncbi.nlm.nih.gov/books/NBK501922/

Detox products and Breastfeeding
I am often asked about products, usually herbal, to detox and about breastfeeding afterwards. In general these products contain a combination of herbal laxatives and at least one diuretic . Basically the result is to make you pass more urine and develop diarrhoea to “cleanse” the system and usually to lose weight. There is a large risk that in doing so your milk supply will diminish too.
The data on the safety of the herbs in breastfeeding is often poor. I cannot provide data that these products are either safe to use and feed as normal or that they are unsafe – there is just is not enough data that I would be confident in using. Therefore I cannot help with information. The decision has to be your own or on the recommendation of a qualified herbalist who is willing to take professional responsibility.

Collagen and breastfeeding
Collagen seems to be another frequent supplement I get asked about . Collagen is found in connective tissue and can be used during exercise routines but also in the prevention and treatment of wrinkles as well as to strengthen hair I believe.
There are no studies on passage into breastmilk and it would therefore be unethical for me to comment.
Elactancia however, designates it as very low risk:
“A fibrous-protein type which is a component of the mammalian connective tissue forming the attachment fibers of all tissues in the organism (bone, cartilage, tendons, skin, muscles, etc.). It represents one-third of total body’s protein content and is composed by amino acids.
Collagen has a great variety of medical, surgical, nutritional and industrial uses such as grafts, sutures, hemostatic products, subcutaneous implants and fillers, pill and capsule covering, glue and cement manufacturing, parts of musical instrument, cosmetic gels, food, photographic and pharmaceutical industry.
Collagen, because of its fibrous nature, is very difficult to chew and digest. To be used as a food it needs to be boiled and treated with various chemicals that break down the bonds and convert it into the so-called hydrolyzed, denatured collagen or gelatin, which is marketed as powder or tablets for various medicinal or health uses like arthritis, joint pains, weight loosing, anti-aging, strengthening of the hair or nails, improvement of the physical fitness and so on, all of them without any serious scientific basis that would guarantee effectiveness.(MedlinePlus Supplements 2015, Revenga 2015, EFSA 2013, EFSA 2011)
Since the last update we have not found any published data on its excretion in breast milk.
Because of a protein nature it is digested by the gastrointestinal tract and absorbed itself as a form of amino acids as those of any other meat. This prevents both the passage to breast milk as a hypothetical plasma absorption by the nursing infant.
Collagen as a supplement is not necessary at all whenever a healthy and balanced diet is followed. https://juanrevenga.com/2015/09/diga-colage-no-o-la-tonteria-de-los-suplementos-de-este-tipo/”
Caffeine and Breastfeeding
Several questions have come up recently about caffeine intake and breastfeeding. With spending more time indoors we are probably all drinking more caffeinated beverages.
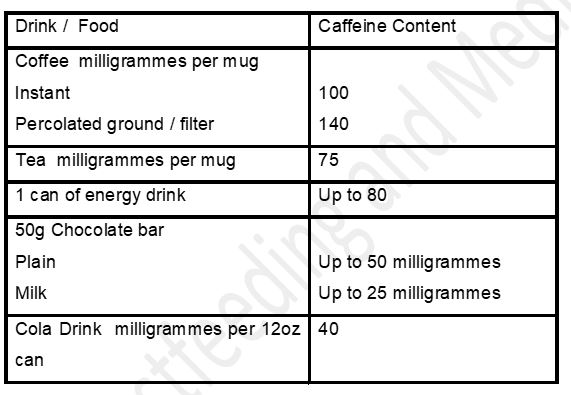
Most of us drink caffeine in one form or another. Women who drink a significant amount of caffeinated drinks who notice that their babies are jittery and restless, may find reduction in caffeine consumption leads to resolution of symptoms. This does not mean that all breastfeeding women need to restrict their consumption of tea and coffee A baby who appears restless may benefit from lowered caffeine intake by the mother but for the average consumption there is little evidence to support restricting intake. From research maternal consumption below 300 milligrammes a day should not cause issues for breastfed babies.
Extract reproduced from Breastfeeding and Medication 2018 by Jones W (Routledge, London)
See also https://www.e-lactancia.org/breastfeeding/caffeine/product/
Moderate coffee consumption does not produce significant levels of caffeine in plasma or urine of infants, and may be undetectable or below therapeutic levels in the neonatal period. (Blanchard 1992, Fulton 1990, Berlin 1984, Hildebrandt 1983, Bailey 1982, Rivera 1977)
Doses greater than 300 – 500 mg of caffeine daily can cause nervousness, irritability and insomnia in the infant (Santos 2012, Martin 2007, Clement 1989, Rustin 1989), as well as decreased iron levels in breast milk and anemia in the infant (Muñoz 1988). Also has been related to the Raynaud’s phenomenon in the nipple of nursing women. (McGuinness 2013)
One study found no problems in infants whose mothers consumed 500 mg of caffeine daily for 5 days. (Ryu 1985)
There is insufficient evidence on the recommended amount of caffeine during lactation. (McCreedy 2018)





